The structure of the pelvis. Female pelvis (bone pelvis)
The pelvic bones, sacrum, coccyx and their ligaments form the pelvis (pelvis). Its upper section is the large pelvis (pelvis major), wide, and is part abdominal cavity, is limited laterally by the wings of the iliac bones, posteriorly by the fifth lumbar vertebra and the lumboiliac ligament, the anterior wall is formed by muscles (Fig. 37). Downwards, the large pelvis passes into the small pelvis (pelvis minor). The plane separating them, called the superior pelvic aperture, is limited by the protrusion of the sacrum, an arcuate line ilium, the crest of the pubic bone and the upper edge of the pubic symphysis. The walls of the small pelvis are: in front - the symphysis, in the back - the sacrum and coccyx, on the sides - the pelvic bones and their ligaments. The inferior pelvic aperture, or its outlet, is limited by the coccyx, the sacrotuberous ligament, the ischial tuberosity, the rami of the ischium and pubis, and the inferior margin of the symphysis.
Like other bone cavities, the pelvis protects the internal organs located in it (rectum, bladder, in women - ovaries, the fallopian tubes, uterus, vagina, and in men - prostate and seminal vesicles). The mechanical significance of the bony ring of the pelvis is great. The heaviness of the head and torso is transmitted through the sacrum and pelvic bones to the lower limbs. In this case, the sacrum and pelvic bones act as a strong arch. In addition to this, the bony pelvis is directly related to one of the essential functions body - childbirth. Therefore, there are significant differences in the structure of the pelvis of men and women.
Sex differences in the structure of the pelvis (Fig. 38; see Fig. 37). Female pelvis lower and wider, while the male one is taller and narrower. The wings of the ilium in women are turned to the sides, while in men they are located more vertically. In men, the pelvic cavity narrows downwards. In the area of the superior aperture, the promontory of the sacrum sharply protrudes forward, the pelvic cavity is narrowed by closely located ischial spines and tuberosities, the symphysis is narrow, high, the exit from the small pelvis is also limited by the protruding coccyx. In general, the pelvic cavity in men seems to be compressed from the sides. In the female pelvis, on the contrary, the entrance to the small pelvis looks like a smooth transverse oval, the promontory of the sacrum does not protrude, the ischial tuberosities are further apart, the symphysis is low, wide, the sacrum is flat, the coccyx gently protrudes into the lumen of the exit from the small pelvis. In general, the small pelvis has the appearance of a wide cylinder. Lower branches pubic bones in women they form a wide arc, and in men - sharp corner. During pregnancy, the fibrous cartilage of the interpubic disc loosens, the cartilage itself and the cavity in it increase, the symphysis becomes wider, which further increases internal cavity small pelvis. Many bony points of the pelvis can be palpated on a living person (iliac crests, superior anterior iliac spines, symphysis, ischial tuberosities, etc.). This makes it possible to obtain the dimensions of the large and small pelvis that are important for obstetric practice. They are determined with a special obstetric caliper-pelvis meter.
Dimensions of a woman's large pelvis (Fig. 39). The spinous distance (distantia spinarum) is 25 - 27 cm. To determine it, the legs of the compass are placed on the upper anterior iliac spines.
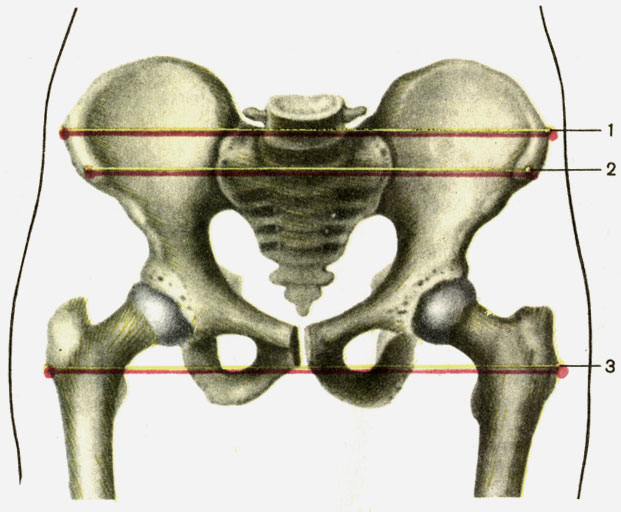
The ridge distance (distantia cristarum) is 28 - 29 cm. The legs of the compass are located at the most distant points of the iliac crests.
The trochanteric distance (distantia trochanterica) is 30 - 32 cm. This is the distance between the greater trochanters of the femurs.
Dimensions of a woman’s pelvis (Fig. 40). The anteroposterior dimensions in the female pelvic area are called direct dimensions or conjugates.
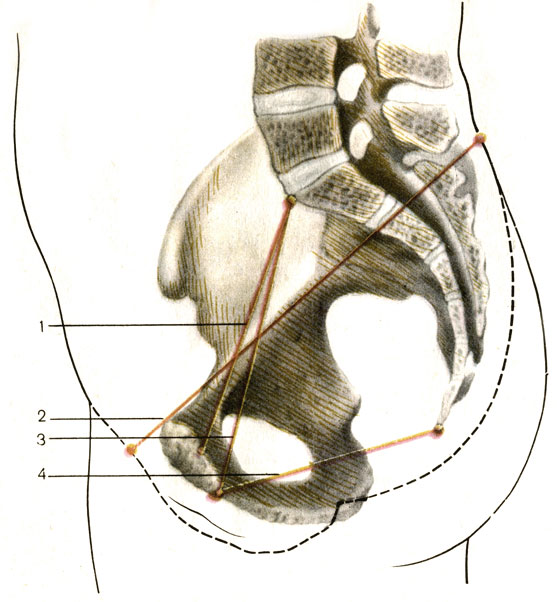
The external conjugate, or external direct size, is 21 cm. To determine it, one leg of the compass is placed on the skin in the area of the upper edge of the pubic symphysis, and the other on the skin in the fossa between the last lumbar and first sacral vertebrae.
A very important true, or obstetric, conjugate (conjugata vera). It characterizes the smallest direct size of the entrance to the small pelvis: between the promontory of the sacrum and the most posteriorly protruding point of the pubic symphysis. On average, a true conjugate is 10.5 - 11.0 cm. It can be determined in two ways. The first method is to subtract 10 cm from the outer direct size (21 cm). The second method involves vaginal examination. In this case, the distance between the promontory of the sacrum and the lower edge of the pubic symphysis is determined. Subtract 2 cm from the resulting figure (12.5 - 13.0 cm).
The direct size of the pelvic outlet is on average 10 cm.
To determine it, one leg of the compass is placed on the skin in the coccyx area, and the other on the lower edge of the symphysis. Subtract 2 cm from the resulting figure (12 cm).
The transverse size of the entrance is 13.5 - 15.0 cm. It is found indirectly: the value of the ridge distance is divided in half.
The transverse size of the outlet from the pelvis is 11 cm (see Fig. 38). The legs of the compass are placed on the inner edges of the ischial tuberosities. To the resulting figure (9 - 10 cm) add 1.0 - 1.5 cm (correction for the thickness of soft tissues).
Pelvis as a whole divided into large and small along the border through the sacral promontory (formed by the anterior part of the base of the sacrum and the body of Y lumbar vertebra), through the arcuate lines of the iliac bones, the crests of the pubic bones and the upper edge of the pubic symphysis - the entire border is called the border line. The pelvic cavity is occupied by internal organs and muscles, and is limited from below by the pelvic and genitourinary diaphragms. The muscles of the lower girdle are located outside the pelvis.
IN pelvis distinguish: an upper aperture (entrance), a cavity with wide and narrow parts, a lower aperture (exit). The upper aperture coincides with the border line, the lower one passes from behind through the apex of the coccyx, on the sides - through the sacrotuberous ligaments, ischial tuberosities, sciatic branches, in front - along the edge of the lower pubic rami and the lower edge of the pubic symphysis. On the anterior wall of the small pelvis there are obturator foramina with the same canals, on the side walls there are large and small sciatic foramina, limited by the same bone notches and sacrotuberous, sacrospinous ligaments.
Age-related differences in the structure of the pelvis are determined by changes in the angle of inclination and degree of curvature of the sacrum and coccyx. Individual fluctuations in the angle of the pelvis (for men - within 50-55 o, for women - 55-60 o) vary depending not only on gender, but also on body position. In a sports or military stance, the angle of inclination increases as much as possible, while in a sitting position it decreases as much as possible. Significant age-related fluctuations are also observed in the timing of ossification of the bones of the pelvic ring.
Sex differences are manifested in the following:
· the female pelvis, and especially its cavity, is wide and low, with a cylindrical shape; male – narrow and tall with a conical cavity;
· the promontory in women protrudes weakly into the cavity, forming an oval-shaped entrance; the promontory in men protrudes strongly, forming an entrance in the form of a card heart;
· the female sacrum is wide and short with a slightly concave, almost flat pelvic surface; male – narrow and long, strongly curved along the pelvic surface;
· subpubic angle in women – more than 90 degrees, in men – 70-75 o;
· the wings of the ilium in women are more turned outward, and in men they have a more vertical position;
· the linear dimensions of the female pelvis prevail over those of men.
In the large pelvis in women, there are three transverse and one longitudinal dimensions:
interspinous size, as direct distance 23-25 cm between the anterior superior iliac spines;
· intercrestal size, as a direct distance of 26-28 cm between the most distant points of the iliac crests;
· intertrochanteric size, as a direct distance of 30-33 cm between the most distant points of the greater trochanters;
· longitudinal dimension, such as a straight distance of 18-21 cm between spinous process Y lumbar vertebra and the upper edge of the pubic symphysis.
All dimensions of the large pelvis are measured with a thick compass in a living woman, since the indicated bone formations easily palpable. By the size of the large pelvis and its shape, one can indirectly judge the shape of the small pelvis.
In the small pelvis there are transverse, oblique, longitudinal dimensions(diameters), which in each part of the pelvis (upper, lower apertures, cavity) are also measured between certain bone landmarks. So, for example, the transverse diameter of the entrance is the distance of 12-13 cm between the most distant points of the arcuate line on the iliac bones; oblique diameter - the distance of 12 cm between the sacroiliac joint of one side and the iliopubic eminence opposite side; the direct size is 11 cm, as the distance between the promontory and the most posteriorly projecting point of the pubic symphysis. The direct outlet size of 9 cm is the distance between the apex of the coccyx and the lower edge of the pubic symphysis; the transverse size of the outlet is 11 cm - the distance between the ischial tuberosities. If you connect the midpoints of all direct dimensions, you will get a wire axis of the small pelvis - a flat curve, concavely facing the symphysis. This is the direction of movement of the born child.
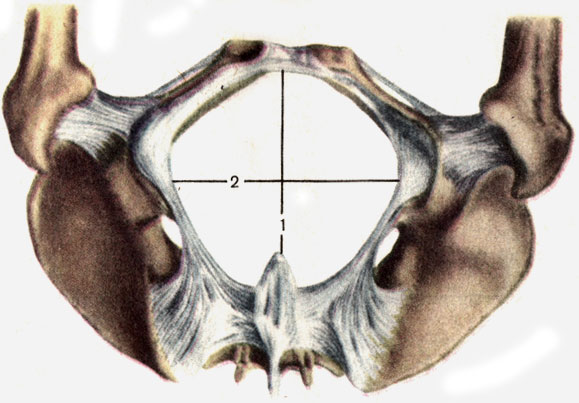
The hip joint is formed by the acetabulum of the pelvic bone and the femoral head. To increase the articular surface along the edge acetabulum There is a fibrocartilaginous acetabular labrum with a transverse acetabular ligament. The articular capsule, consisting of fibrous and synovial membranes, is attached along the edge of the acetabular lip, and on femur along the neck: in front - along the intertrochanteric line, behind - inward from the intertrochanteric ridge. The capsule is strengthened by powerful ligaments: the orbicularis zone, the iliofemoral, pubic and ischiofemoral ligaments. Inside the joint there is a ligament of the head of the femur, which during its formation holds the head in the socket.
The shape of the hip joint is spherical, triaxial, appearing as a variety of these joints - a cup-shaped joint. Around the frontal axis, flexion is performed in it with the knee bent at 118-121 o, with the knee extended - only at 84-87 o due to tension posterior muscles hips. Flexion is carried out by the muscles: iliopsoas, rectus femoris, sartorius, pectineus, tensor fasciae lata. They are supplied with blood by the following arteries: the iliopsoas, superior gluteal, obturator, external genital, deep and lateral surrounding ilium, descending knee, muscular branches of the femoral and deep femoral arteries. Innervation is carried out by branches of the lumbar plexus, obturator, femoral and superior gluteal nerves
Knee-joint.
In education knee joint Three bones are involved: the femur with articular condylar surfaces, the patella with the posterior articular surface, the tibia with the upper articular surfaces on the medial and lateral condyles. Therefore, the joint is complex and condylar with insufficient correspondence of the articulating surfaces, which is complemented by fibrocartilaginous menisci: medial and lateral. This makes the joint complex.
The medial meniscus is narrow, semilunar (shaped like the letter “ WITH"); lateral meniscus – wide, oval (shaped like the letter “ ABOUT"). In front, both menisci are connected by the transverse ligament of the knee; internally they grow to the intercondylar eminence of the tibia. The thin and loose capsule fuses with the outer edges of the menisci, its synovial membrane forms large wing-shaped and numerous small folds filled with adipose tissue, which increases congruence articular surfaces. Paired pterygoid folds lie on the sides and downwards of the patella. The patellar fold - unpaired - is located below the patella, located between it and the anterior intercondylar field.
The synovial membrane in the joint forms pockets (sines, volvulus), the size and number of which are variable. Synovial bursae arise in the places of attachment of muscle tendons: suprapatellar (the most extensive), subpatellar deep, popliteal pocket (behind - at the tendon of the muscle of the same name), bursa of the sartorius tendon, subcutaneous prepatellar bursa. Some bags, connecting to the joint cavity, increase its volume.
The joint capsule is strengthened by internal and external ligaments. The internal ligaments include the cruciate ligaments: anterior and posterior, filling the intercondylar fossa of the femur and the intercondylar field of the tibia. The extra-articular, external ligaments include: the tibial and fibular collaterals lying on the sides, behind - the oblique popliteal and arcuate popliteal, in front - the patellar ligament (patellar) and the medial and lateral suspensory ligaments of the patella.
The knee joint is a typical condylar joint, complex and complex, and the following movements are performed in it:
· around the frontal axis: flexion and extension with a range of 140-150 o; flexion is inhibited by the cruciate ligaments and the quadriceps tendon; the condyles of the femur slide along the menisci;
· around the longitudinal (vertical) axis the volume of active rotation is on average 15 o, passive - 30-35 o; inward rotation is limited cruciate ligaments, outwards - collateral ligaments.
Joints of the leg bones.
Tibia
The distal epiphysis has:
Fibula It has:
The bones of the lower leg have connections:
· tibiofibular joint, formed by the flat articular surfaces of the fibular head and the upper epiphysis (lateral part), the tibia; the articular capsule is tightly stretched and strengthened by the anterior and posterior ligaments of the head of the fibula; limited range of motion; sometimes the tibiofibular joint can communicate with the cavity of the knee joint;
· tibiofibular syndesmosis – continuous connection short and thick fibrous fibers between the fibular notch on the distal epiphysis of the tibia and the articular surface of the lateral malleolus, strengthened by the anterior and posterior tibiofibular ligaments, the synovial membrane of the ankle joint is invaginated into the tibiofibular syndesmosis;
· interosseous membrane of the leg– a fibrous membrane stretched between the interosseous edges of the tibia and fibula in the area of their diaphysis; it has openings at the top and bottom for the passage of blood vessels and nerves.
There is almost no movement in the joints of the lower leg bones, which is associated with the supporting function of the lower limb and the formation of a mobile ankle joint.
· tibia
· fibula
· talus
Tibia on the proximal epiphysis has:
· medial and lateral condyles with articular surfaces;
· intercondylar eminence with medial and lateral tubercles: anterior and posterior field;
· fibular articular surface on the lateral side below the condyle.
On the diaphysis of the tibia are located:
· anterior edge (sharp) – upward passes into the tuberosity, lateral edge facing the fibula and medial edge;
· surfaces: medial, lateral and posterior with the line of the soleus muscle.
The distal epiphysis has:
· fibular notch along the lateral edge;
medial malleolus with posterior malleolar groove;
· articular surfaces: ankle and lower.
Ossification nuclei in the tibia appear in the proximal epiphysis at the end of the fetal period, in the distal epiphysis - in the 2nd year of life, in the diaphysis - at the beginning of the fetal period. Final ossification occurs at 19-24 years, ankles - at 16-19 years.
Fibula It has:
· on the proximal epiphysis the head, neck, on the head – the apex and articular surface;
· on the diaphysis: anterior, posterior and interosseous edges; lateral, posterior and medial surfaces;
· on the distal epiphysis: the lateral malleolus with the articular surface and fossa (posteriorly).
Secondary ossification nuclei appear in the distal epiphysis at the 2nd year of life, in the proximal epiphysis at 3-5 years, and final ossification occurs at 20-24 years.
Ankle joint.
The following are involved in the formation of a joint:
· the tibia with its inferior and medial malleolar articular surfaces;
The fibula is the articular surface of the lateral malleolus;
· talus with superior and malleolar (medial and lateral) articular surfaces located on the trochlea;
· the ankles wrap around the block in a fork-like manner, forming a typical trochlear joint - complex due to the articulation of three bones.
The articular capsule is attached at the back along the edge of the articular surfaces of the bones that make up the joint, at the front 0.5-1 cm above it.
On the sides the capsule is thick and strong, in front and behind it is thin, loose, folded; reinforced by lateral ligaments:
· medial(deltoid) - thick, strong, fanning out from the medial malleolus to the talus, navicular and calcaneus; the ligament has parts: tibiofanavicular, tibiocalcaneal, anterior and posterior tibiotalar;
· lateral as part of the anterior talofibular, posterior talofibular, calcaneofibular ligaments.
The ligaments are so strong, especially the medial one, that with maximum stretching they can tear off the ankle.
The following movements are performed in the ankle and talocalcaneal-navicular joints:
· bending(plantar) and extension (sometimes called dorsiflexion) around the frontal axis with a span of 60 degrees;
· adduction and abduction around sagittal axis with a span of 17 degrees;
· pronation and supination around a vertical axis with a span of 22 degrees.
Foot joint.
Foot bones divided into tarsal bones: 7 short spongy bones and metatarsal bones consisting of 5 short tubular bones; as well as phalanges of fingers - three in each finger, except for the first, which has two phalanges. The tarsal bones lie in two rows: in the proximal (posterior) - talus and calcaneus, in the distal (anterior) - scaphoid, sphenoid: medial, intermediate, lateral and cuboid bones.
Talus consists of body, head, neck. On top of the body there is a block with the upper, medial and lateral malleolar articular surfaces. Below the body are the heel articular surfaces: anterior, middle and posterior. There is a groove between the middle and posterior heel surfaces talus. On the head lies the scaphoid articular surface. The talus has processes: lateral and posterior, on the latter there are medial and lateral tubercles, separated by a groove for the tendon of the long flexor pollicis.
Calcaneus has a body ending posteriorly with a calcaneal tubercle. There are talar articular surfaces on the body: anterior, middle and posterior. There is a groove between the middle and back calcaneus, which, together with the groove of the talus, forms the sinus of the tarsus. At the distal end of the body there is a cuboidal articular surface. Processes and other grooves of the calcaneus - supporting process of the talus on the medial surface, groove of the long tendon peroneus muscle on the lateral surface.
Scaphoid at the distal end it has three articular surfaces for the sphenoid bones, and a tuberosity along the medial edge for the attachment of the tibialis posterior muscle.
Sphenoid bones have a characteristic triangular shape, and on the front and back sides and on the sides there are articular surfaces - in the front for articulation with the first three metatarsal bones, in the back for connection with the scaphoid bone, on the sides for articulation between themselves and the cuboid bone.
Cuboid also has articular surfaces at the back for articulation with the heel, and at the front with metacarpal bones, and along the medial surface - to connect the lateral sphenoid and scaphoid bones. On the lower surface there is a tuberosity and a groove for the tendon of the peroneus longus muscle.
Bones of the metatarsus and phalanges of the fingers- these are short tubular bones, each of which consists of a base, body and head. The articular surfaces are located on the head and base. The head of the first metatarsal bone is divided from below into two platforms, with which the sesamoid bones are in contact. On the lateral surface of the Y metatarsal there is a tuberosity for the attachment of the peroneus brevis muscle. Each distal (nail) phalanx ends in a tubercle for the attachment of muscle tendons.
Primary ossification nuclei appear in the calcaneus at the 6th month of the fetal period, in the talus - at 7-8, in the cuboid - at the 9th month. In the remaining bones of the tarsus, secondary nuclei are formed: in the lateral sphenoid - at the 1st year, in the medial sphenoid - at 3-4 years, in the scaphoid - at 4-5 years, complete ossification - at 12-16 years.
Metatarsal bones begin to ossify in the epiphyses at 3-6 years, complete ossification - at 12-16 years. Diaphyses of phalanges and metatarsal bones Primary nuclei form at 12-14 weeks of the fetal period, secondary nuclei - in the phalanges - at 3-4 years, complete ossification of the phalanges - at 18-20 years
The formation of the ankle joint involves:
· tibia its inferior and medial malleolar articular surfaces;
· fibula- articular surface of the lateral malleolus;
· talus- upper and ankle (medial and lateral articular surfaces), located on the block.
The ankles fork around the trochlea, forming a typical trochlear joint, complex due to the articulation of three bones.
The articular capsule is attached at the back along the edge of the articular surfaces of the articulating bones, at the front 0.5-1 cm above it.
On the sides the capsule is thick and strong, in front and behind it is thin, loose, folded, reinforced by powerful lateral ligaments:
· medial (deltoid) – thick, strong, fanning out from the medial malleolus to the talus, navicular and calcaneus; the ligament has parts: tibiofanavicular, tibiocalcaneal, anterior and posterior tibiotalar;
· lateral as part of the anterior talofibular, posterior talofibular, calcaneofibular ligaments.
The ligaments are so strong, especially the medial one, that with maximum stretching they can tear off the ankle.
IN ankle joint movements performed:
· bending(plantar) and extension (dorsiflexion) around the frontal axis with a span of 60 o;
· adduction and abduction around the sagittal axis with a span of 17 o;
· pronation and supination around a vertical axis with a span of 22 o.
Subtalar joint formed by the posterior articular surfaces of the talus and calcaneus, which correspond well to each other. The capsule at the joint is thin, stretched, and strengthened by ankle ligaments.
Talocaleonavicular joint formed by the articular surface on the head of the talus, which articulates in front with the scaphoid bone, and below with the calcaneus. The articular surface of the calcaneus is supplemented by the plantar calcaneonavicular ligament, which at the head of the talus becomes fibrocartilage. The articular capsule is attached along the edge of the articular surfaces, closing a single cavity. The capsule is strengthened by strong ligaments: the interosseous talocalcaneal ligament, up to 0.5 cm thick, and the talonavicular ligament on top. When they are stretched (especially the talocalcaneal ligament), the head of the talus descends and the foot flattens.
The joint is spherical in shape, but with one sagittal axis of movement. Together with the subtalar it makes up combined joint with a limited range of movements in the form of adduction and abduction, rotation of the foot outward and inward. The total volume of all movements does not exceed 55 degrees. In a newborn and infant this joint is in a supinated position; with the beginning of walking, pronation gradually occurs with the lowering of the medial edge of the foot.
Calcaneocuboid joint– saddle-shaped with high congruence of articular surfaces; joint capsule with medial side thick and taut, on the lateral side – thin and loose, strengthened by ligaments: plantar calcaneocuboid and long plantar. Movements in a limited volume are carried out around the longitudinal axis in the form of a slight rotation, complementing the movements in the talocaleonavicular joint.
The transverse (Schopar) tarsal joint includes the calcaneocuboid and talonavicular joints so that the joint space takes on the appearance of a Latin S, running across the foot. The common ligament of joints is bifurcated ( lig. bifurcatum) - serves as a kind of key, when cut, the joint cavity opens wide. It is Y-shaped and consists of the calcaneonavicular and calcaneocuboid ligaments.
Wedge-navicular joint– flat, complex, as it is formed by three sphenoid and one scaphoid bones, strengthened by the dorsal and plantar sphenonavicular and intra-articular intersphenoid ligaments. The joint cavity can communicate with the tarsometatarsal joints.
Tarsometatarsal (Lisfranc) joints– flat with limited range of motion, include the following three joints:
joint between the medial cuneiform and first metatarsal bones;
· joint between intermediate, lateral sphenoid bones and II, III metatarsals;
· joint between the cuboid bone and IY, Y metatarsal bones;
· the tarsometatarsal joints are strengthened by tarso-metatarsal ligaments (dorsal and plantar) and interosseous cuneotarsal ligaments, of which the medial cuneotarsal ligament is considered in practice to be the key to these joints.
Intermetatarsal joints– flat, formed by the lateral surfaces of the bases of the metatarsal bones, reinforced by the dorsal and plantar metatarsal interosseous ligaments. Movement in them is severely limited.
Metatarsophalangeal joints formed by the spherical heads of the metatarsal bones and the concave bases of the proximal phalanges. The capsules are thin, loose, reinforced by collateral and plantar ligaments. The deep transverse metatarsal ligament connects the heads of the metatarsal bones and strengthens the joint capsules. Flexion and extension in them is 90°, adduction and abduction are limited.
Interphalangeal joints– proximal and distal, except for the thumb joint, where one interphalangeal joint. They belong to the trochlear joints, strengthened by collateral and plantar ligaments.
The human foot has lost the adaptations of the prehensile organ, but has acquired arches necessary for support and movement of the entire body.
The tarsal and metatarsal bones are connected to each other by inactive joints.
Moreover, due to the shape of the bones and their “tight” joints, five longitudinal and one transverse arches convex upward were formed with support points on the calcaneal tubercle and the heads of the I and Y metatarsal bones.
The longitudinal arches run along the long axis of the metatarsal bones: from their heads, through the body to the base and then through the adjacent tarsal bones to the calcaneal tubercle, where they all converge. The longest and highest is the second arch.
The medial longitudinal arches perform a springing function, the lateral arches perform a supporting function. At the most high points The longitudinal arches are crossed by a transverse arch.
The arches are held in place due to the shape of the bones and joints, strengthened by passive “tightenings” - ligaments with the plantar aponeurosis and active “tightenings” - muscles and their tendons. The longitudinal arches strengthen the following ligaments: long plantar, calcaneonavicular and plantar aponeurosis. Transverse arch support metatarsal transverse and interosseous ligaments. The tendons of the long flexor and extensor muscles of the fingers, the tibial muscles, as well as the short flexor muscles of the fingers, and the lumbrical muscles strengthen the longitudinal arches. The transverse arch is held in place by the quadratus plantae, adductor and interosseous muscles.
During the process of human evolution, major changes occurred in the foot related to its arched structure. Three supporting points were formed on the sole - the heel and the bases of the first and fifth toes, the tarsal bones increased in size, and the phalanges of the toes were significantly shortened. The joints of the foot became stiff. Attachment of long muscles of the leg and short muscles the foot has shifted in the medial direction towards thumb, which increases pronation of the foot and strengthens the arches. The loss of acquired properties is accompanied by the development of flat feet, which is a disease for humans.
Page 3 of 6
pelvis as a whole
Pelvis(pelvis) formed by the connecting pelvic bones and the sacrum. It is a bone ring (Fig. 111). The pelvis is a container for many internal organs. With the help of the pelvic bones, the torso is connected to the lower limbs. There are two sections - the large and small pelvis.
Big pelvis(pelvis major) is delimited from the lower pelvis by a border line. Border line(linea terminalis) passes through the promontory of the sacrum, along the arcuate lines of the iliac bones, the crests of the pubic bones and the upper edge of the pubic symphysis. The large pelvis is limited from behind by the body of the V lumbar vertebra, from the sides by the wings of the ilium. The large pelvis does not have a bony wall in front.
Small pelvis(pelvis minor) is limited posteriorly by the pelvic surface of the sacrum and the ventral surface of the coccyx. On the side, the walls of the pelvis are the inner surface of the pelvic bones (below the boundary line), the sacrospinous and sacrotuberous ligaments. The anterior wall of the pelvis is the upper and lower branches of the pubic bones, the pubic symphysis.
The small pelvis has an inlet and an outlet. Upper aperture (opening) of the pelvis(apertura pelvis superior) is limited by the border line. Exit from the pelvis - inferior pelvic outlet(apertura pelvis inferior) is limited behind by the coccyx, on the sides by the sacrotuberous ligaments, the branches of the ischial bones, the ischial tuberosities, the lower branches of the pubic bones, and in front by the pubic symphysis. The obturator foramen, located in the lateral walls of the pelvis, is closed by fibrous tissue. obturator membrane(membrana obturatoria). Spreading over the obturator groove, the membrane limits obturator canal(canalis obturatorius). Vessels and a nerve pass through it from the pelvic cavity to the thigh. In the lateral walls of the pelvis there are also large and small sciatic foramina. Greater sciatic foramen(foramen ischiаdicum majus) is limited by the greater sciatic notch and the sacrospinous ligament. Lesser sciatic foramen(foramen ischiаdicum minus) is formed by the lesser sciatic notch, sacrotuberous and sacrospinous ligaments.
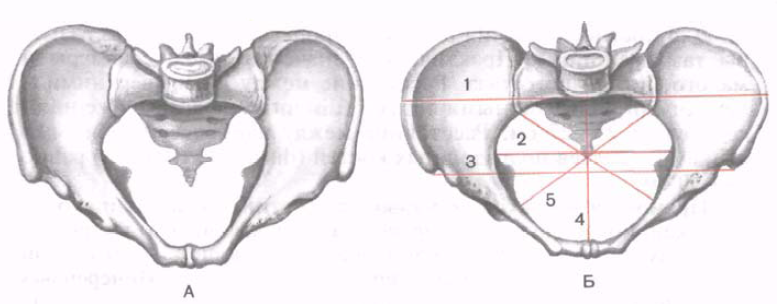
Rice. 111. Male (A) and female (B) pelvis. The lines of the dimensions of the large pelvis and the entrance to the small pelvis are indicated. 1 - distаntia cristаrum (distance between the iliac crests); 2 - transverse diameter; 3 - distantia spinаrum (distance between the anterior superior iliac spines); 4 - true (gynecological) conjugate; 5 - oblique diameter.
The structure of the pelvis is related to a person’s gender. The superior aperture of the pelvis vertical position the body of women forms an angle of 55-60° with the horizontal plane (Fig. 112). The pelvis in women is lower and wider, the sacrum is wider and shorter than in men. The promontory of the sacrum in women protrudes less forward. Ischial tuberosities more turned to the sides, the distance between them is greater than in men. The angle of convergence of the lower branches of the pubic bones in women is 90° (pubic arch), in men it is 70-75° (subpubic angle).
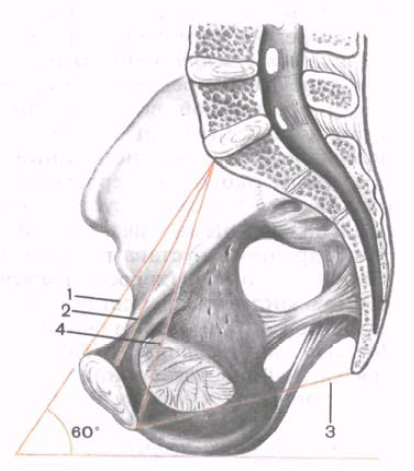
Rice. 112. Dimensions of the female pelvis. (Cut in the sagittal plane.) 1 - anatomical conjugate; 2 - true (gynecological) conjugate; 3 - straight size (outlet from the pelvis); 4 - diagonal conjugate; 60° - pelvic tilt angle.
For forecasting birth process It is important to know the size of a woman’s pelvis. Practical significance They have the sizes of both small and large pelvis. Distance between the two top and front iliac spines(distаntia spinаrum) in women is 25-27 cm. The distance between the most distant points of the wings iliac bones(distantia cristarum) is 28-30 cm.
Direct size of the inlet to the pelvis ( true, or gynecological, conjugate- conjugata vera, s. gynaecologica) is measured between the promontory of the sacrum and the most posteriorly projecting point of the pubic symphysis. This size is 11 cm. The transverse diameter (diameter transvеrsa) of the entrance to the pelvis - the distance between the most distant points of the border line - is 13 cm. Oblique diameter(diameter obliqua) of the entrance to the small pelvis is 12 cm. It is measured between the sacroiliac joint of one side of the pelvis and the iliopubic eminence of the other side.
1. TOPIC OF THE CLASS: PELVIS FROM AN OBSTETRIC POINT OF VIEW: DIMENSIONS OF THE LARGE PELVIS, SMALL PELVIS, ITS PLANES AND SIZES. THE FETUS AS AN OBJECT OF BIRTH: FETAL HEAD, SKULL BONES, SUTURES AND fontanelles. SIZES OF THE HEAD OF A FULL FETUS. POSITION OF THE FETUS IN THE UTERUS.
2. Form of organization of the educational process: practical lesson.
3. Theme meaning(relevance of the problem being studied): Knowledge of anatomical formations, the size of a normal pelvis, and the average size of the fetus is necessary for further study of obstetrics.
4. Learning objectives:
4.1. common goal: study of the anatomy of the pelvis and structural features of the fetus; obstetric terminology.
4.2. Learning objective: the student must know the structure of the woman’s pelvis and the fetal head; carry out measurements of the pelvis and head of the fetus, as well as timely diagnose deviations in the structure and size of the pelvis.
4.3. Psychological and pedagogical goal: Knowledge of the anatomical features of the structure of the bony pelvis allows the doctor to determine the tactics of pregnancy and childbirth.
The student must know:
structure of the bony pelvis;
pelvic planes, their boundaries and sizes, diagonal, anatomical and true conjugates;
wire axis and pelvic inclination angle;
muscles and fascia pelvic floor;
the structure of the skull of a full-term fetus, sutures, fontanelles and the dimensions of the head, shoulder and pelvic girdle of the fetus;
basic obstetric terms (articulation, position, fetal axis, presentation, position and appearance);
signs of pregnancy (doubtful, probable, reliable), methods for diagnosing pregnancy, hormonal tests.
The student must be able to:
show on a model of the female pelvis the boundaries of the planes of the small pelvis, identifying points of the anatomical and true conjugate;
four ways to determine with vera;
show the sutures and fontanelles on the head of a full-term fetus (doll);
size of the head of a full-term fetus, signs of full term;
on a phantom, give the doll a certain position, position, appearance, presentation;
determine the gestational age using various methods.
5. Place of practical training: pregnancy pathology department, maternity ward, training room, methodological room.
6. Lesson equipment:
1. Tables
2. A set of tickets to control the initial level of knowledge of students.
3. A set of tickets for monitoring the final knowledge of students.
4. Obstetric simulator with a doll.
5. Dummy bone pelvis.
6. Model “Doll”.
7. Tazometer, measuring tape.
8. Obstetric stethoscope.
8. Topic abstract(summary)
Of great importance in obstetrics is the bony pelvis, which forms the solid foundation of the birth canal. The pelvic floor, stretching, is included in the birth canal and promotes the birth of the fetus.
Female pelvis (bone pelvis)
Bone pelvis is a durable container for the female internal genital organs, rectum, Bladder and surrounding tissues. The woman's pelvis forms the birth canal through which the emerging fetus moves. The development and structure of the pelvis has great importance in obstetrics.
The pelvis of a newborn girl differs sharply from the pelvis of an adult woman, not only in size, but also in shape. The sacrum is straight and narrow, located vertically, the promontory is almost absent, its area is located above the plane of the entrance to the pelvis. The entrance to the small pelvis has an oval shape. The wings of the ilium stand steeply, the pelvis narrows significantly towards the outlet. As the body develops, the volume and shape of the pelvis changes. The development of the pelvis, as well as the entire organism as a whole, is determined by environmental conditions and hereditary factors. The formation of the pelvis in childhood is particularly influenced by influences associated with sitting, standing, and walking. When a child begins to sit, the pressure of the trunk is transmitted to the pelvis through the spinal column. When standing and walking, pressure on the pelvis from above is added to pressure from the lower extremities. Under the influence of pressure from above, the sacrum moves somewhat into the pelvis. There is a gradual increase in the pelvis in the transverse direction and a relative decrease in the anteroposterior dimensions. In addition, the sacrum, under the influence of pressure from above, rotates around its horizontal axis so that the promontory descends and begins to protrude into the entrance to the pelvis. In this regard, the entrance to the pelvis gradually takes on the shape of a transverse oval with a notch in the area of the promontory. When the sacrum is rotated around a horizontal axis, its apex should move posteriorly, but it is held in place by the tension of the sacrospinous and sacrotuberous ligaments. As a result of the interaction of these forces, a curvature of the sacrum (sacral cavity) is formed, typical of the pelvis of an adult woman.
Differences between the female and male pelvis begin to appear during puberty and become distinct in adulthood:
1. the bones of the female pelvis are thinner, smoother and less massive than the bones of the male pelvis;
2. the female pelvis is lower, wider and larger in volume;
3. the sacrum in women is wider and not as strongly concave as in the male pelvis;
4. The sacral promontory in women protrudes forward less than in men;
5. the symphysis of the female pelvis is shorter and wider;
6. the entrance to the pelvis in a woman is wider, the shape of the entrance is transverse-oval, with a notch in the promontory area; the entrance to the male pelvis resembles a card heart due to the sharper protrusion of the promontory;
7. The pelvic cavity in women is larger, its outlines approaching a cylinder curved anteriorly; the cavity of the male pelvis is smaller, it narrows funnel-shaped downwards;
8. the outlet of the female pelvis is wider because the distance between the ischial tuberosities is greater, the pubic angle is wider (90-100 0) than in men (70-75 0); The tailbone protrudes anteriorly less than in the male pelvis.
Thus, the female pelvis is more voluminous and wider, but less deep than the male pelvis. These features are important for the birth process.
The process of pelvic development can be disrupted under unfavorable conditions of intrauterine development associated with diseases, poor nutrition and other disorders in the mother’s body. Severe debilitating diseases and unfavorable living conditions in childhood and puberty can lead to delayed development of the pelvis. IN similar cases features characteristic of the child and adolescent pelvis can persist until the woman reaches puberty.
PELVIC BONES
The pelvis consists of four bones: two pelvic (or innominate), the sacrum and the coccyx.
Pelvic (nameless) bone(os coxae, os innominatum) up to 16-18 years old consists of three bones connected by cartilage: ilium, pubis and ischium. After ossification of the cartilages, these bones fuse together, forming the innominate bone.
Ilium(os ilium) consists of two parts: the body and the wing. The body makes up the short, thickened part of the ilium and participates in the formation of the acetabulum. The wing of the ilium is a fairly wide plate with a concave inner and convex outer surface. The thickest free upper edge of the wing forms iliac crest(crista iliaca). In front, the ridge begins with a protrusion ( anterosuperior spine- spina iliaca anterior superior), below is the second protrusion (anteroinferior spine - spina iliaca anterior inferior). Under the anteroinferior axis, at the junction with the pubic bone, there is a third eminence - iliopubic tubercle(tuberculum iliopubicum). Between the anterosuperior and anterioinferior iliac spine there is the lesser iliac notch, and between the anterosuperior and anteroinferior iliac spine there is the greater iliac notch. The iliac crest ends posteriorly posterosuperior iliac spine(spina iliaca posterior superior), below which there is a second protrusion - the posteroinferior iliac spine (spina iliasa posterior inferior). Under the posteroinferior spine is the greater sciatic notch (incisura ischiadica major). On the inner surface of the ilium, in the area where the wing meets the body, there is a comb-like protrusion that forms an arched border, or nameless line (linea terminalis, s innominata). This line runs from the sacrum across the entire ilium, and in front passes to the upper edge of the pubic bone.
Ischium(os ischii) has a body involved in the formation of the acetabulum, and two branches: upper and lower. Upper branch goes from the body down and ends ischial tuberosity(tuber ischiadicum). On the back surface of the lower branch there is a protrusion - ischial spine(spina ischiadica). The lower branch is directed anteriorly and upward and connects with the lower branch of the pubic bone.
pubic bone, or pubic (os pubis), forms the anterior wall of the pelvis. The pubic bone consists of a body and two branches: superior (horizontal) and inferior (descending). The short body of the pubis forms part of the acetabulum, the lower ramus connects to the corresponding ramus of the ischium. On the upper edge of the superior (horizontal) branch of the pubic bone there is a sharp ridge, which ends in front with the pubic tubercle (tuberculm pubicum). The upper and lower rami of both pubic bones are connected to each other in front through a sedentary pubic symphysis (joint) - symphysis(symphisis). Both pubic bones are connected at the symphysis by intermediate cartilage, in which there is often a small slit-like cavity filled with fluid; During pregnancy, this gap increases. The lower rami of the pubic bones form an angle under the symphysis called the pubic arch. The connecting branches of the pubic and ischial bones limit a rather large obturator foramen (foramen obturatorium).
Sacrum(os sacrum) consists of five fused vertebrae. The size of the sacral vertebrae decreases downwards, so the sacrum has the shape of a truncated cone. The wide part of it - the base of the sacrum - faces upward, the narrow part - the apex of the sacrum - faces down. The posterior surface of the sacrum is convex, the anterior one is concave, it forms the sacral cavity. On the anterior surface of the sacrum (on the cavity) four transverse rough lines are noticeable, corresponding to the ossified cartilaginous joints of the sacral vertebrae. The base of the sacrum (surface of the 1st sacral vertebra) articulates with the 5th lumbar vertebra; a protrusion forms in the middle of the anterior surface of the base of the sacrum - sacral promontory(promontorium). Between the spinous process of the V lumbar vertebra and the beginning of the middle sacral crest, it is possible to palpate the depression ( suprasacral fossa), which is used when measuring the pelvis.
Coccyx(os coccygis) consists of 4-5 fused vertebrae, is a small bone, tapering downward.
The pelvic bones are connected through the symphysis, sacroiliac and sacrococcygeal joints. Cartilaginous layers are located in the joints of the pelvis. The joints of the pelvis are strengthened by strong ligaments. Symphysis is a sedentary joint, a semi-joint.
There are two sections of the pelvis: the upper - large pelvis - and the lower - small pelvis. The boundaries between the large and small pelvis are: in front - the upper edge of the symphysis and pubic bones, on the sides - the innominate lines, in the back - the sacral promontory. The plane lying between the large and small pelvis is the plane of entry into the small pelvis; this plane is of utmost importance in obstetrics.
BIG PELIN
The large pelvis is much wider than the small one; it is limited on the sides by the wings of the ilium, behind by the last lumbar vertebrae, and in front by the lower abdominal wall. The volume of the large pelvis can change in accordance with the contraction or relaxation of the abdominal muscles. The large pelvis is available for research; its dimensions are determined quite accurately. The size of the large pelvis is used to judge the size of the small pelvis, which cannot be directly measured. Determining the size of the small pelvis has important, since the born fetus passes through the stubborn bony canal of the small pelvis.
Usually four sizes of the pelvis are measured: three transverse and one straight.
1. Distantia spinarum (24-26 cm)
2. Distantia cristarum (27-29 cm)
3. Distantia trochanterica (30-31 cm)
4. Conjugata externa (20-21 cm)
By the size of the external conjugate, one can judge the size of the true conjugate: 9 cm is subtracted from the length of the external one. The sacral rhombus (Michaelis rhombus) is also examined and measured.
SMALL PELVIS
Determining the size of the small pelvis is important because... The newborn fetus passes through the stubborn bony canal of the small pelvis. The small pelvis has: an inlet, a cavity and an outlet. In the pelvic cavity there are wide and narrow parts.
Planes and dimensions of the small pelvis. The pelvis is a bony part birth canal. The posterior wall of the pelvis consists of the sacrum and coccyx, the lateral ones are formed by the ischial bones, and the anterior wall is formed by the pubic bones and the symphysis. The posterior wall of the pelvis is 3 times longer than the anterior one. Upper section The pelvis is a continuous, inflexible ring of bone. In the lower section, the walls of the small pelvis are not solid; they contain obturator foramina and sciatic notches, bounded by two pairs of ligaments (sacrospinous and sacrotuberous).
In the small pelvis there are the following sections: inlet, cavity and outlet. In the pelvic cavity there are a wide and a narrow part. In accordance with this, four planes of the pelvis are considered: I – the plane of the entrance to the pelvis, II – the plane of the wide part of the pelvic cavity, III – the plane of the narrow part of the pelvic cavity, IV – the plane of the exit of the pelvis.
I. Plane of entry into the pelvis has the following boundaries: in front – the upper edge of the symphysis and the upper inner edge of the pubic bones, on the sides – innominate lines, in the back – the sacral promontory. The entrance plane has the shape of a kidney or a transverse oval with a notch corresponding to the sacral promontory. At the entrance to the pelvis there are three sizes: straight, transverse and two oblique.
Straight size– the distance from the sacral promontory to the most prominent point on the inner surface of the symphysis pubis. This size is called the obstetric, or true, conjugate (conjugata vera). There is also an anatomical conjugate - the distance from the promontory to the middle of the upper inner edge of the symphysis; the anatomical conjugate is slightly (0.3-0.5 cm) larger than the obstetric conjugate. Obstetric, or true conjugate is 11 cm.
Transverse size– the distance between the most distant points of nameless lines. This size is 13-13.5 cm.
Oblique sizes two: right and left, which are equal to 12-12.5 cm. The right oblique dimension is the distance from the right sacroiliac joint to the left iliopubic tubercle, the left oblique dimension is from the left sacroiliac joint to the right iliopubic tubercle. In order to more easily navigate in the direction of the oblique dimensions of the pelvis in a woman in labor, M.S. Malinovsky and M.G. Kushnir is offered next appointment. The hands of both hands are folded at right angles, with the palms facing upward; the ends of the fingers are brought closer to the outlet of the pelvis of the lying woman. The plane of the left hand will coincide with the left oblique size of the pelvis, the plane of the right hand will coincide with the right.
II. The plane of the wide part of the pelvic cavity has the following boundaries: in front - the middle of the inner surface of the symphysis, on the sides - the middle of the acetabulum, in the back - the junction of the II and III sacral vertebrae. In the wide part of the pelvic cavity, two sizes are distinguished: straight and transverse.
Straight size– from the junction of the II and III sacral vertebrae to the middle of the inner surface of the symphysis; equals 12.5 cm.
Transverse size– between the apices of the acetabulum; equals 12.5 cm.
There are no oblique dimensions in the wide part of the pelvic cavity because in this place the pelvis does not form a continuous bone ring. Oblique dimensions in the widest part of the pelvis are conditionally allowed (length 13 cm).
III. The plane of the narrow part of the pelvic cavity bounded in front by the lower edge of the symphysis, on the sides by the spines of the ischial bones, and behind by the sacrococcygeal joint. There are two sizes: straight and transverse.
Straight size goes from the sacrococcygeal joint to the lower edge of the symphysis (apex of the pubic arch); equal to 11-11.5 cm.
Transverse size connects the spines ischium; equals 10.5 cm.
IV. Pelvic exit plane has the following boundaries: in front - the lower edge of the symphysis, on the sides - the ischial tuberosities, in the back - the apex of the coccyx. The pelvic exit plane consists of two triangular planes, common ground which is the line connecting the ischial tuberosities. There are two sizes at the outlet of the pelvis: straight and transverse.
Straight pelvic outlet size goes from the top of the coccyx to the lower edge of the symphysis; it is equal to 9.5 cm. When the fetus passes through the small pelvis, the tailbone moves away by 1.5-2 cm and the direct size increases to 11.5 cm.
Transverse size of the pelvic outlet connects the inner surfaces of the ischial tuberosities; equal to 11 cm. Thus, at the entrance to the pelvis, the largest dimension is the transverse one. In the wide part of the cavity, the straight and transverse dimensions are equal; the largest size will be the conventionally accepted oblique size. In the narrow part of the cavity and the pelvic outlet, the straight dimensions are larger than the transverse ones.
Wired axis (line) of the pelvis. All planes (classical) of the pelvis border in front with one or another point of the symphysis, and in the back - with different points of the sacrum or coccyx. The symphysis is much shorter than the sacrum and coccyx, so the planes of the pelvis converge anteriorly and fan out posteriorly. If you connect the middle of the straight dimensions of all the planes of the pelvis, you will get not a straight line, but a concave anterior (towards the symphysis) line. This conditional line connecting the centers of all direct dimensions of the pelvis is called the wire axis of the pelvis. The wire axis of the pelvis is initially straight; it bends in the pelvic cavity according to the concavity of the inner surface of the sacrum. In the direction of the wire axis of the pelvis, the born fetus passes through the birth canal.
The angle of inclination of the pelvis (the intersection of the plane of its entrance with the plane of the horizon) when a woman is standing can vary depending on the body type and ranges from 45-55 0 . It can be reduced by forcing a woman lying on her back to strongly pull her thighs towards her stomach, which leads to elevation of the womb. It can be increased by placing a roll-shaped hard pillow under the lower back, which will lead to a downward deviation of the womb. A decrease in the angle of inclination of the pelvis is also achieved if the woman is given a semi-sitting position, squatting.
PELVIC FLOOR
The outlet of the pelvis is closed from below by a powerful muscular-fascial layer, which is called the pelvic floor. The part of the pelvic floor located between the posterior commissure of the labia and the anus is called the obstetric or anterior perineum (the posterior perineum is the part of the pelvic floor located between the anus and the tailbone).
The pelvic floor consists of three layers of muscles covered by fascia:
I. Bottom (outer) layer consists of muscles converging in the tendon center of the perineum; the shape of these muscles resembles a figure eight suspended from the pelvic bones.
1. Bulbocavernosus muscle(m.bulbo-cavernosus) wraps around the entrance to the vagina, attaches to the tendon center and the clitoris; when contracted, this muscle compresses the vaginal opening.
2. Ischiocavernosus muscle(m.ischio-cavernosis) starts from the lower branch of the ischium and attaches to the clitoris.
3. Superficial transverse perineal muscle(m.transversus perinei superficialis) starts from the tendon center, goes to the right and left, attaches to the ischial tuberosities.
4. External sphincter of the anus(m.sphincter ani externus) is a muscle surrounding the end of the rectum. Deep bundles of muscles of the external sphincter of the anus begin at the top of the coccyx, wrap around the anus and end in the tendon center of the perineum.
II. Middle layer of pelvic muscles– the urogenital diaphragm (diaphragma urogenitale) occupies the anterior half of the pelvic outlet. The urogenital diaphragm is a triangular muscular-fascial plate located under the symphysis, in the pubic arch. The urethra and vagina pass through this plate. IN anterior section urogenital diaphragm - muscle bundles surround the urethra and form its external sphincter; in the posterior section there are muscle bundles running in the transverse direction to the ischial tuberosities. This part of the urogenital diaphragm is called the deep transverse perineal muscle. (m.transversus perinei profundus).
III. Upper (inner) The layer of muscles of the perineum is called the pelvic diaphragm (diaphragma pelvis). The pelvic diaphragm consists of a paired muscle that lifts the ani (m.levator ani). Both vastus levator muscles anus, form a dome, the top of which faces down and is attached to lower section rectum (slightly above the anus). The wide base of the dome faces upward and is attached to the inner surface of the walls of the pelvis. In the anterior section of the pelvic diaphragm, between the bundles of muscles that lift the ani, there is a longitudinally located gap through which the urethra and vagina (hiatus genitalis) exit the pelvis. The levator ani muscles consist of separate muscle bundles starting from various parts of the pelvic walls; This layer of the pelvic muscles is the most powerful. All pelvic floor muscles are covered by fascia.
During childbirth, the perineum is often injured, and it is the inner layer pelvic floor.
The muscles and fascia of the pelvic floor perform the following essential functions:
1. The pelvic floor is a support for the internal genital organs and helps maintain their normal position. The levator ani muscles are of particular importance. When these muscles contract, the genital fissure closes, narrowing the lumen of the rectum and vagina. Damage to the pelvic floor muscles leads to prolapse and prolapse of the genitals.
2. The pelvic floor provides support not only for the genitals, but also for the insides. The pelvic floor muscles are involved in the regulation of intra-abdominal pressure together with the thoraco-abdominal barrier and the muscles of the abdominal wall.
3. During childbirth, when the fetus is expelled, all three layers of the pelvic floor muscles stretch and form a wide tube, which is a continuation of the bone birth canal. After the birth of the fetus, the pelvic floor muscles contract again and return to their previous position.









