How bones are connected. Introduction, Types of bones. Types of bone connections - Musculoskeletal system
Continuous connections have greater elasticity, strength and, as a rule, limited mobility. Depending on the type of tissue connecting the bones, there are three types of continuous connections:
1) fibrous compounds,
2) synchondrosis (cartilaginous joints)
3) bone connections.
Fibrous connections
Articulationes fibrosae, are strong bone connections using dense fibrous connective tissue. Three types of fibrous joints have been identified: syndesmoses, sutures and impactions.
|
|
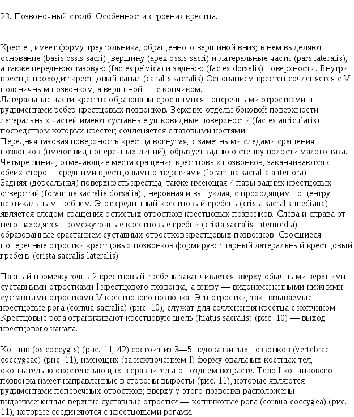
Types of bone connections (diagram).
A-joint. B-syndesmosis. B-synchondrosis. G-symphysis (hemiarthrosis). 1 - periosteum; 2 - bone; 3 - fibrous connective tissue; 4 - cartilage; 5 - synovial membrane; 6- fibrous membrane; 7 - articular cartilage; 8-articular cavity; 9-slit in the interpubic disc; 10-interpubic disc.
Syndesmosis, syndesmosis, is formed by connective tissue, the collagen fibers of which fuse with the periosteum of the connecting bones and pass into it without a clear boundary. Syndesmoses include ligaments and interosseous membranes. Ligaments, ligamenta, are thick bundles or plates formed by dense fibrous connective tissue. For the most part, ligaments spread from one bone to another and reinforce discontinuous joints (joints) or act as a brake that limits their movement. In the spinal column there are ligaments formed by elastic connective tissue that has yellowish color. Therefore, such ligaments are called yellow, ligamenta flua. The yellow ligaments are stretched between the vertebral arches. They stretch when bent spinal column anteriorly (flexion of the spine) and, due to their elastic properties, are shortened again, promoting extension of the spinal column.
Interosseous membranes, membranae interosseae, are stretched between the diaphyses of long tubular bones. Often, interosseous membranes and ligaments serve as the origin of muscles.
A suture, sutura, is a type of fibrous joint in which there is a narrow connective tissue layer between the edges of the connecting bones. The connection of bones by sutures occurs only in the skull. Depending on the configuration of the edges of the connecting bones, a serrated suture, sutura serrata, is distinguished; scaly suture, sutura squamosa, and flat suture, sutura plana. In a serrated suture, the jagged edges of one bone fit into the spaces between the teeth of the edge of another bone, and the layer between them is connective tissue. If the connecting edges flat bones have obliquely cut surfaces and overlap each other in the form of scales, a scaly seam is formed. In flat sutures, the smooth edges of two bones are connected to each other using a thin connective tissue layer.
A special type of fibrous joint is impaction, gomphosis (for example, dentoalveolar joint, articulatio dentoalueolaris). This term refers to the connection of the tooth with the bone tissue of the dental alveolus. Between the tooth and the bone there is a thin layer of connective tissue - periodontium, periodontum.
Synchondroses, synchondroses, are bone joints with the help of cartilage tissue. Such joints are characterized by strength, low mobility, and elasticity due to the elastic properties of cartilage. The degree of bone mobility and the amplitude of springing movements in such a joint depend on the thickness and structure of the cartilaginous layer between the bones. If the cartilage between the connecting bones exists throughout life, then such synchondrosis is permanent. In cases where the cartilaginous layer between the bones persists until a certain age (for example, sphenoid-occipital synchondrosis), this is a temporary connection, the cartilage of which is replaced by bone tissue. Such a joint replaced by bone tissue is called a bone joint - synostosis, synostosis (BNA).
DISCONTINUOUS OR SYNOVIAL JOINTS OF BONES (JOINTS)
Synovial joints (joints),
articulationes synoviales are the most advanced types of bone connections. They are distinguished by great mobility and a variety of movements. Each joint includes articular surfaces of bones covered with cartilage, an articular capsule, an articular cavity with a small amount of synovial fluid. Some joints also have auxiliary formations in the form of articular discs, menisci and articular labrum.
Articular surfaces, fades articulares, in most cases, the articulating bones correspond to each other - they are congruent (from the Latin congruens - corresponding, coinciding). If one articular surface is convex (articular head), then the second, articulating with it, is equally concave (glenoid cavity). In some joints these surfaces do not correspond to each other either in shape or size (incongruent).
Read more >>>
Nursing process in the work of district nurses with peptic ulcer disease
"In the circle of victims peptic ulcer Increasingly, these are young people, and even teenagers. The results of prevention and treatment of this disease do not satisfy either doctors or patients. The social cost of the disease is still...
Endocrinology (molecular mechanisms of insulin secretion and its action on cells)
Insulin is a polypeptide hormone formed by 51 amino acids. It is secreted into the blood by the b cells of the islets of Langerhans in the pancreas. Main function insulin - regulation of protein metabolism,...
Tissue repair and cancer transformation
The purpose of this abstract is to compare two processes - the process of malignant tissue degeneration and the process of reparative regeneration. At first glance, they have nothing in common, although this is probably...
The role of the nurse manager in organizing treatment and care for patients with mental disorders
The role of the nurse leader in the organization healing process and care for mental patients is difficult to overestimate, since it includes a wide range of issues, without which it would be impossible to care for...
Chapter 5 BONE JOINTS
5.1. General arthrosyndesmology
The literal translation of the term “arthrosyndesmology” means “the study of joints and ligaments.” In a generalized view, arthrosyndesmology is the science of bone joints.
There are two main types of bone joints - continuous and discontinuous (joints). In addition, there is a special type of bone joints - symphyses (half-joints).
Continuous connections. There are three groups of continuous bone connections: fibrous, cartilaginous and osseous.
Fibrous connections- connections using connective tissue (syndesmoses), which include ligaments, membranes, fontanelles, sutures and impactions.
Ligaments- these are compounds that look like bundles of collagen and elastic fibers that provide bone fixation.
Membranes- connections that look like an interosseous membrane, filling large spaces between the bones and separating groups of antagonist muscles.
fontanelles- these are connections between the bones of the skull in the fetus, newborn and child of the first year of life, having the shape of a membrane.
Seams- these are thin layers of connective tissue containing a large number of collagen fibers, located between the bones of the skull. The fontanelles and sutures serve as a growth zone for the bones of the skull and have a shock-absorbing effect.
Injections- connection of the roots of the teeth with the cells of the alveolar processes of the jaws using dense connective tissue, which has a special name - periodontium. The periodontium provides fixation and shock absorption of the tooth and participates in the nutrition of its tissues.
Cartilage joints (synchondrosis). These compounds are represented by hyaline or fibrous cartilage. Based on the duration of their existence, synchondrosis is classified into permanent and temporary.
Temporary joints are mainly represented by hyaline cartilage, which exists until a certain age and is then replaced by bone tissue. Temporary synchondrosis includes: metaepiphyseal cartilage (cartilaginous layers between the epiphyses and diaphyses of tubular bones), hyaline cartilage between parts of the pelvic bone, hyaline cartilage between parts of the bones of the base of the skull.
Permanent cartilage is mainly represented by fibrous cartilage. Permanent synchondrosis are intervertebral discs, sternocostal synchondrosis (1st ribs), and costal arch.
Connections using bone tissue(synostosis). Under normal conditions, temporary synchondroses, fontanelles, and sutures undergo synostosis. These are physiological synostoses. In some diseases (bechterew's disease, osteochondrosis, etc.), ossification can occur not only in synchondrosis, but also in syndesmoses, and even in joints. These are pathological synostoses.
Symphyses (half-joints). This is an intermediate type between discontinuous and continuous connections. The symphyses are cartilage located between two bones, in which there is a small cavity without the synovial lining inherent in the articular cavity. An example of this connection is the pubic symphysis, symphysis pubica. Symphyses are formed at the connection of the bodies of the V lumbar and I sacral vertebrae, as well as between the sacrum and coccyx.
Intermittent connections. These are joints or synovial joints. A joint, articulatio, is a discontinuous, cavity-like connection formed by articulating articular surfaces covered with cartilage, enclosed in an articular capsule (capsule), which contains synovial fluid.
The joint includes three main elements: the articular surfaces, covered with cartilage; joint capsule; joint cavity.
Articular surfaces- These are areas of bone covered with articular cartilage. More often, the articular surfaces are lined with hyaline (vitreous) cartilage. Fibrous cartilage covers the articular surfaces of the temporomandibular, sternoclavicular, acromioclavicular and sacroiliac joints. Articular cartilage prevents bones from fusing with each other, prevents bone destruction (withstands heavy loads than bone) and ensures the sliding of the articular surfaces relative to each other.
Joint capsule, or bursa, hermetically surrounds the articular cavity. On the outside it is represented by dense connective tissue, and on the inside it is lined synovial membrane, which ensures the formation and absorption of synovial fluid. The joint capsule is strengthened by extra-articular ligaments, which are located in places heaviest load and belong to the fixing apparatus.
Joint cavity- this is a hermetically sealed space, limited by the articular surfaces and capsule, filled with synovial fluid. The latter provides nutrition to the articular cartilage, adhesion (holding) of the articular surfaces relative to each other, and reduces friction during movements.
In addition to the main elements in the joints, there may be auxiliary elements that ensure optimal joint function. The auxiliary elements of the joint are located only in the joint cavity. The main ones are intra-articular ligaments, intra-articular cartilage, articular lips, articular folds, sesamoid bones and synovial bursae.
Intra-articular ligaments- These are ligaments covered with a synovial membrane that connect the articular surfaces. They are found in the knee joint, rib head joint and hip joint.
Intra-articular cartilage- These are fibrous cartilages located between the articular surfaces in the form of a plate, which completely divides the joint into two floors and is called the articular disc. In this case, two separated cavities are formed (in the sternoclavicular and temporomandibular joints). When the joint cavity is only partially divided, i.e. the cartilage plates are shaped like a crescent and their edges are fused with the capsule - these are menisci (in the knee joint).
Articular labrum- This is a ring-shaped fibrous cartilage that complements the articular fossa along the edge. In this case, with one edge the lip fuses with the joint capsule, and with the other it passes into the articular surface. The labrum is located in two joints: the shoulder and the hip.
Articular folds- These are connective tissue formations rich in blood vessels. Folds covered with synovial membrane are called synovial. If fatty tissue accumulates in large quantities inside the folds, then fat folds are formed (pterygoid folds - in the knee joint; fat body acetabulum - in the hip).
Sesamoid bones- These are intercalary bones that are closely connected to the joint capsule and the muscle tendons surrounding the joint. One of their surfaces is covered with hyaline cartilage and faces the joint cavity. The largest sesamoid bone is the patella. Small sesamoid bones are located in the joints of the hand and foot (for example, in the interphalangeal, carpometacarpal joint of the first finger, etc.).
Synovial bursae- these are small cavities lined with synovial membrane, often communicating with the joint cavity. Synovial fluid accumulates inside them, which lubricates nearby tendons.
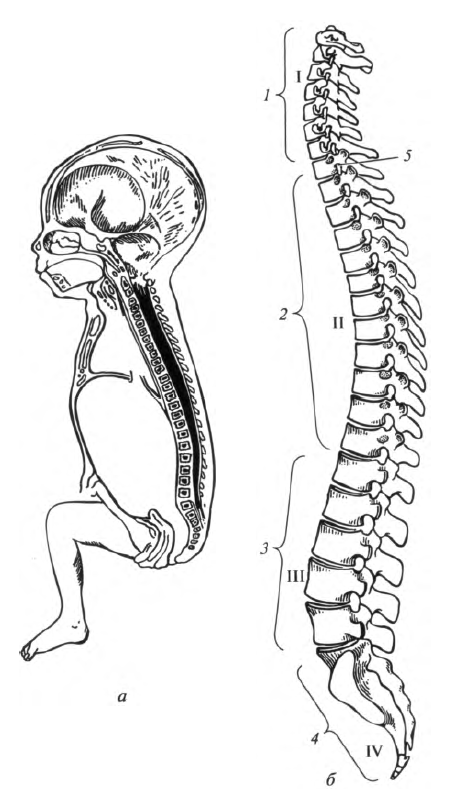
Depending on the shape of the articular surfaces, joints can function around one, two, or three axes (uniaxial, biaxial, and multiaxial joints). The classification of joints according to the shape of the articular surfaces and the number of axes is presented in Table. 5.1.
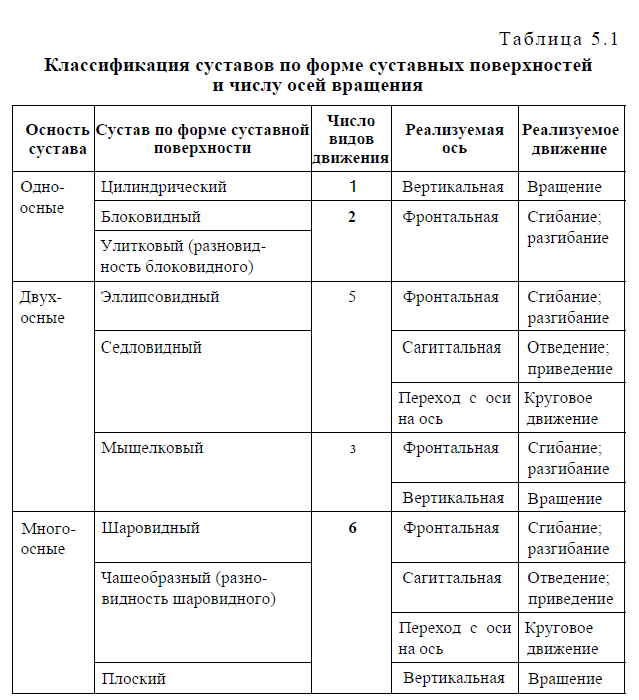 Uniaxial joints- these are joints in which movements are made only around one axis (frontal, sagittal or vertical). The cylindrical and trochlear joints are uniaxial in shape of the articular surfaces (Fig. 5.1). A type of trochlear joint is a cochlear, or helical joint, the notch and ridge of which are beveled and have a helical stroke.
Uniaxial joints- these are joints in which movements are made only around one axis (frontal, sagittal or vertical). The cylindrical and trochlear joints are uniaxial in shape of the articular surfaces (Fig. 5.1). A type of trochlear joint is a cochlear, or helical joint, the notch and ridge of which are beveled and have a helical stroke.
Biaxial joints- joints that function around two axes of rotation. So, if movements are performed around the frontal and sagittal axes, then such joints realize five types of Movement: flexion, extension, adduction, abduction and circular Movement.
The shape of the articular surfaces is ellipsoidal or saddle-shaped. If movements occur around the front axes and vertical axes, it is possible to realize only three types of movement - flexion, extension and rotation. The shape is a condylar joint.
Rice. 5.1. Joint shape: 1 - ellipsoid; 2 - saddle-shaped; 3 - spherical; 4 - block-shaped
Multi-axis joints- these are joints in which movements are carried out around all three axes. They perform the maximum possible number of types of movement - 6. These are spherical joints in shape, for example the shoulder. A type of spherical joint is cup-shaped, or nut-shaped (for example, hip).If the surface of a ball has a very large radius of curvature, then it approaches a flat surface. A joint with such a surface is called a flat joint, for example the sacroiliac joint. However, flat joints are inactive or immobile, since the areas of their articular surfaces are almost equal to each other.
Depending on the number of surfaces forming a joint, the latter are classified into simple and complex.
Simple joint is a joint in the formation of which only two articular surfaces take part, each of which can be formed by one or more bones. For example, the articular surfaces of the interphalangeal joints are formed by only two bones; and in wrist joint The three bones of the proximal carpal row form a single articular surface.
Complex joint- is a joint in one capsule of which there are several articular surfaces, i.e. a few simple joints. The only complex joint is the elbow. Some authors also include the knee joint as a complex joint. We consider the knee joint to be simple, since the menisci and patella are auxiliary elements.
Based on their simultaneous joint function, combined and non-combined joints are distinguished.
Combined joints- these are anatomically separated joints, i.e. located in different joint capsules, but functioning only together. Such joints, for example, are intervertebral, atlanto-occipital, temporomandibular, etc.
When combining joints with various forms articular surfaces, movements are realized along the joint, which has a smaller range of movements. Thus, the lateral atlantoaxial joint is flat, i.e. multiaxial, but since it is combined with the median atlantoaxial joint (cylindrical, uniaxial), they function as a single uniaxial cylindrical joint.
Non-combined joint functions independently.
Factors that determine the range of motion in a joint. It should be noted that the range of motion in the joint depends on a number of factors, the main of which are the following:
1) difference in areas of articulating surfaces - main factor; the greater the difference, the greater the range of movements;
2) the presence of auxiliary elements. For example, the articular labrums, by increasing the articular surface area, help limit movements; intra-articular ligaments limit movement only in a certain direction ( cruciate ligaments the knee joint does not prevent flexion, but counteracts excessive extension);
3) combination of joints: for example, the movements of combined joints are determined by a joint that has a smaller number of axes of rotation (see Table 5.1);
4) the condition of the joint capsule: with a thin, elastic capsule, movements occur in a larger volume;
5) the state of the fixing apparatus: ligaments have an inhibitory effect, since collagen fibers have low extensibility;
6) the muscles surrounding the joint, possessing constant tone, bring together and fix the articulating bones;
7) synovial fluid has an adhesive effect and lubricates the articular surfaces; in metabolic-dystrophic diseases (arthrosis-arthritis), the secretion of synovial fluid is disrupted and pain, crunching appear in the joints, and the volume of movements decreases;
8) Atmosphere pressure promotes contact of articular surfaces, has a uniform tightening effect and moderately limits movement;
9) condition of the skin and subcutaneous fat: for skin diseases ( inflammatory diseases, burns, scars), when it loses elasticity, the range of movements decreases significantly.
5.2. Joints of the trunk bones
The joints of the body bones include the joints of the vertebrae, ribs and sternum.
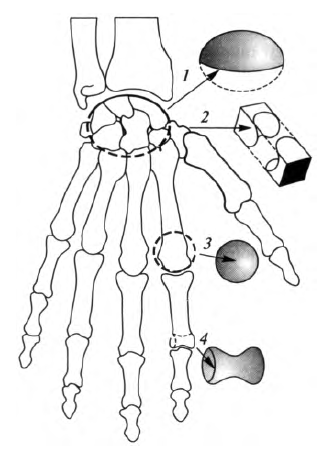
Connections of typical vertebrae. In free typical vertebrae, connections of bodies, arches and processes are distinguished.
The bodies of two adjacent vertebrae are connected by intervertebral discs, disci intervertebrales (Fig. 5.2). The disc consists of two parts: along the periphery there is a fibrous ring, consisting of fibrous cartilage; central part The disc consists of the nucleus pulposus. It consists of an amorphous substance of cartilage and plays the role of an elastic cushion, i.e. serves as a shock absorber.
The vertebral bodies are connected anteriorly and posteriorly by two longitudinal ligaments. The anterior longitudinal ligament runs along the anterior surface of the vertebral bodies from the base of the skull to the first sacral vertebra. The posterior longitudinal ligament is located on the posterior surface of the vertebral bodies from the clivus occipital bone to the sacral canal.
The vertebral arches are connected by the yellow ligaments. They fill the gaps between the arches, leaving free interposes sinkholes.
Rice. 5.2. Vertebral connections: 1 - vertebral body; 2 - intervertebral disc; 3 - anterior longitudinal ligament; 4 - radiate ligament of the rib head; 5 - joint of the rib head; 6 - superior articular process; 7 - transverse process; 8 - intertransverse ligament; 9 - spinous process; 10 - interspinous ligaments; 11 - supraspinous ligament; 12 - lower articular process; 13 - intervertebral foramen
Between two adjacent spinous processes there are short interspinous ligaments. Posteriorly, they directly pass into the unpaired supraspinous ligament, which runs along the apices of all spinous processes. Between the transverse processes are the intertransverse ligaments. They are absent in the cervical region.
The only continuous connections between the vertebrae are the intervertebral joints. The lower articular processes of each overlying vertebra articulate with the upper articular processes of the underlying vertebra. The articular surfaces of the processes are flat, covered with hyaline cartilage; The articular capsule is attached along the edge of the articular surfaces. In terms of function, these are multi-axial, combined joints. They allow the body to tilt forward and backward (flexion and extension), to the sides, circular movement, torsion movement, or twisting, and slight springing movements.
The fifth lumbar vertebra articulates with the sacrum using the same connections that are characteristic of free typical vertebrae.
The bodies of the 5th sacral and 1st coccygeal vertebrae are connected by an intervertebral disc, inside of which in most cases there is a small cavity. In this case, this connection is called the symphysis. In addition, this joint is strengthened by the sacrococcygeal ligaments.
Connections of the 1st and 2nd cervical vertebrae to each other and to the skull. The atlantooccipital joint, articulatio atlantooccipitalis, paired, is formed by the condyles of the occipital bone and the upper articular surfaces of the first cervical vertebra. The articular surfaces are covered with hyaline cartilage, the capsule is free, attached along the edge of the articular surfaces. The atlanto-occipital joints are ellipsoidal and biaxial. Anatomically, they are separate, but function together (combined joints). They perform nodding movements around the frontal axis: tilting the head forward and backward. Around sagittal axis The head is tilted to the right and left. Peripheral (circular) movement is also possible.
Between the occipital bone and the atlas are the anterior and posterior atlanto-occipital membranes, which extend from the edges of the foramen magnum to the anterior and posterior arches of the atlas.
Between the I (atlas) and II (axial) cervical vertebrae there are three joints: the middle atlantoaxial joint, articulatio atlantoaxialis roediana, the right and left lateral atlantoaxial joints, articulationes atlantoaxiales laterales dextra et sinistra.
Median atlantoaxial joint formed by the tooth of the II cervical vertebra and the articular fossa of the anterior arch of the atlas. The displacement of the tooth is prevented by the transverse ligament of the atlas, stretched behind it between the medial surfaces of the lateral masses. The shape of this joint is cylindrical; movement in it is only possible around vertical axis- turn the head right and left. The rotation of the atlas around the tooth occurs along with the skull.
Lateral atlantoaxial joints formed by the inferior articular surface on the lateral mass of the atlas and the superior articular surface of the axial vertebra. They are flat in shape, and combined in function with each other and with the median atlantoaxial joint. Consequently, movements in the lateral atlantoaxial joints are carried out together with movement in the median atlantoaxial joint, so only one type of movement is possible - rotation.
These joints are strengthened by pterygoid ligaments running from the apex of the tooth to the occipital condyles; the ligament of the apex of the tooth, which is stretched from the apex of the tooth to the anterior edge of the large foramen; anterior and posterior longitudinal ligaments running from the occipital bone along the body of the axial vertebra down to the sacrum. The latter, together with the transverse ligament of the atlas, form the cruciate ligament.
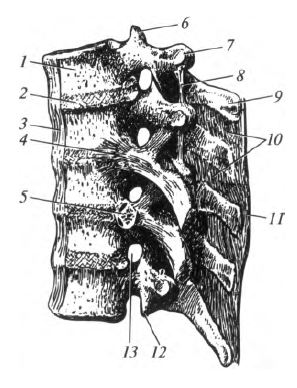
The spinal column or spine, columna vertebralis, is represented by vertebrae and their joints. It includes the cervical, thoracic, lumbar, sacral and coccygeal regions (Fig. 5.3). The functional significance of the spine is extremely great: it supports the head, serves as a flexible axis of the body, takes part in the formation of the walls of the chest and abdominal cavities and pelvis, serves as a support for the body, protects spinal cord located in the spinal canal.
The spinal column does not occupy a strictly vertical position. It has physiological bends in sagittal plane. Curves facing convexly backward are called kyphosis, kyphosis (thoracic and sacral), while curves facing forward are called lordosis, lordosis (cervical and lumbar). At the junction V lumbar vertebra with the I sacral there is a significant protrusion - a promontory.
The formation of the curves of the spinal column occurs after birth. In a newborn, the spinal column looks like an arch, convexly facing backwards. At 2 - 3 months of age, the child begins to hold his head up, and cervical lordosis forms. At 5-6 months of age, when he begins to sit up, characteristic shape acquires thoracic kyphosis. At 9-12 months of age, lumbar lordosis forms as a result of the human body adapting to a vertical position (the child begins to walk). At the same time, an increase in thoracic and sacral kyphosis occurs. Normally, the spinal column has no bends in the frontal plane. Its deviation from the median plane is called “scoliosis.”
The movements of the spinal column are the result of the functioning of numerous combined joints between the vertebrae.
Rice. 5.3. Curvatures of the spinal column: a - spinal column of a newborn; b - spinal column of an adult; I - cervical lordosis; II - thoracic kyphosis; III - lumbar lordosis; IV - sacral kyphosis; 1 - cervical vertebrae; 2 - thoracic vertebrae; 3 - lumbar vertebrae; 4 - sacrum and coccyx; 5 - intervertebral foramen
In the spinal column, when skeletal muscles act on it, it is possible the following types movements: bending forward and backward, to the sides; torsional movements, i.e. twisting; circular (conical) and springing movements.The volume and types of movements realized in each part of the spinal column are not the same. Cervical and lumbar regions most mobile due to the greater height of the intervertebral discs. The thoracic part of the spinal column is the least mobile, which is due to the lower height of the intervertebral discs, the strong downward inclination of the spinous processes of the vertebrae, as well as the frontal location of the articular surfaces in the intervertebral joints.
Rib connections. The ribs form connections with the thoracic vertebrae, the sternum and with each other.
The ribs are connected to the vertebrae by costovertebral joints. These include the rib head joint and the costotransverse joint.
rib head joint, articulatio capitis costae, formed by the costal fossae of the thoracic vertebral bodies and the head of the corresponding rib. These joints are saddle-shaped or spherical in shape. Externally, the joint capsule is strengthened by the radiate ligament (see Fig. 5.2). Its bundles fan out and attach to the intervertebral disc and to the bodies of adjacent vertebrae.
Costotransverse joint, articulatio costotransversaria, formed by the tubercle of the rib and the costal fossa of the transverse process. It is cylindrical in shape (rotational). Since the rib head joint and the costotransverse joint are combined, they function only as rotational joints.
The ribs are connected to the sternum using discontinuous and continuous connections. The cartilage of the first rib fuses directly with the sternum, forming a permanent synchondrosis. The cartilages of the II-VII ribs are connected to the sternum using the sternocostal joints, articulationes stemocostales. They are formed by the anterior ends of the costal cartilages and costal notches on the sternum.
The anterior ends of the false ribs (VIII, IX and X) are not directly connected to the sternum, but form a costal arch. Their cartilages are connected to each other, and sometimes there are modified intercartilaginous joints between them. These arches limit the substernal angle. The short cartilaginous ends of the XI and XII ribs end in the muscles of the abdominal wall.
The anterior ends of the ribs are connected to each other externally intercostal membrane. In the posterior sections of the intercostal spaces, the internal intercostal membrane is well defined.
Functionally, the joint of the rib head, the costotransverse joint and the sternocostal joints are combined into a uniaxial rotational joint. The rear end of the rib rotates around its own axis, while its front end rises or falls. When the anterior ends of the ribs are raised, the volume of the chest increases, which, together with the lowering of the diaphragm, provides inhalation. Exhalation occurs as the ribs lower due to relaxation of the muscles and elasticity of the costal cartilages.
The chest as a whole. The chest, thorax, consists of 12 thoracic vertebrae, 12 pairs of ribs, the sternum and their joints. It forms the walls of the chest cavity, which contains internal organs: heart, lungs, trachea, esophagus, etc.
The shape of the chest is compared to a truncated cone, the base of which faces downwards. The anterior-posterior size of the chest is smaller than the transverse one. The anterior wall is the shortest, formed by the sternum and costal cartilages. Side walls the longest, they are formed by the bodies of twelve ribs. Back wall presented thoracic region spinal column and ribs.
Up chest cavity opens with a wide opening - the upper aperture of the chest, which is limited by the manubrium of the sternum, I pair of ribs and the body of I thoracic vertebra. The lower aperture of the chest is much wider than the upper one, it is limited by the body of the XII thoracic vertebra, XII pair ribs, ends of the XI pair of ribs, costal arches and the xiphoid process.
The spaces located between adjacent ribs are called intercostal spaces. They are filled with intercostal muscles, ligaments and membranes.
Vessels, nerves, trachea and esophagus pass through the upper aperture of the chest. The lower opening of the chest is closed by the diaphragm. Depending on the body type, there are three shapes of the chest: conical, cylindrical and flat. The conical shape of the chest is characteristic of the mesomorphic body type, cylindrical - dolichomorphic and flat - brachymorphic.
5.3. Connections of the skull bones
The bones of the skull are connected to each other mainly through continuous connections. Only the temporomandibular joint is a discontinuous joint.
In an adult, the bones of the roof of the skull are connected by sutures. The shape is distinguished between jagged, scaly and flat seams. Serrated sutures are located between the parietal bones (sagittal suture); between the parietal and frontal (coronal suture); between the parietal and occipital (lambdoid suture). The scales are connected using a scaly suture temporal bone with the parietal bone and the greater wing of the sphenoid bone. The bones of the facial skull are connected through flat (harmonic) sutures. The names of the sutures are made up of the names of the connecting bones, for example: frontozygomatic, zygomaticomaxillary, etc.
In the skull of a fetus, a newborn and a child of the first two years of life, in addition to flat sutures, there are fontanelles (see subsection 4.3).
Cartilaginous joints - synchondrosis - are characteristic of the bones of the base of the skull of children. As a person ages, cartilage is replaced by bone tissue.
Temporomandibular joint, articulatio temporomandibularis, - condylar, combined joint. It is formed by the head lower jaw, mandibular fossa and articular tubercle of the temporal bone (Fig. 5.4). The articular surfaces are lined with fibrous cartilage.
The peculiarity of the temporomandibular joint is the presence of an articular disc, which ensures congruence of the articular surfaces. The anterior part of the joint capsule is thinner. Over the entire surface, the capsule has fused with the articular disc, as a result of which the joint cavity is separated into upper and lower floors. WITH outside it is strengthened by the lateral ligament.
The following types of movements are possible in the temporomandibular joint: 1) around the frontal axis - lowering and raising the lower jaw; moving the lower jaw forward and moving back while simultaneously shifting this axis; 2) around a vertical axis - rotation.
When the lower jaw is lowered, the head slides forward and, with the maximum opening of the mouth, comes out onto the articular tubercle. If the lower jaw is lowered excessively, its dislocation is possible - moving anteriorly from the articular tubercle. When extending the lower In the jaw, the condylar processes, together with the articular discs, slide forward and extend onto the tubercles in both joints.
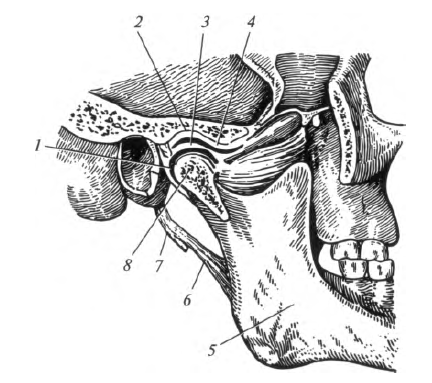
Rice. 5.4. Temporomandibular joint: 1 - joint capsule; 2 - mandibular fossa; 3 - articular disc; 4 - articular tubercle; 5 - lower jaw; 6 - stylomandibular ligament; 7 - styloid process; 8 - head of the lower jaw
When rotating the lower jaw in the right and left joints, the movements are different. In this case, in one joint (towards which the movement occurs) rotation occurs in the fossa, in the other - the head, together with its disk, comes out onto the tubercle, moving in a circle.5.4. Bone connections upper limb
Connections of the bones of the upper limb girdle. They can be divided into three groups.
1. Connections of the bones of the belt to each other. The acromioclavicular joint, articulatio acromioclavicularis, is formed between the acromion and the clavicle. The joint capsule is tight, strengthened by the acromioclavicular ligament. Additionally, the joint is secured by the coracoclavicular ligament. The joint is practically motionless.
2. The proper connections of the scapula are represented by the coracoacromial and superior transverse ligaments. The coracoacromial ligament runs from the tip of the acromion to the coracoid process. It forms the “arch of the shoulder joint”, protecting the joint from above and limiting the movement of the humerus in this direction. The superior transverse scapular ligament is stretched over the notch of the scapula.
3. Connections between the bones of the belt and the skeleton of the body. Between the clavicle and the manubrium of the sternum there is the sternoclavicular joint, articulatio stemoclavicularis, which is formed by the sternal end of the clavicle and the clavicular notch of the manubrium of the sternum (Fig. 5.5). The articulating surfaces are covered with fibrous cartilage and have a saddle shape. An intra-articular disc is located in the joint cavity. The collarbone moves up and down around the sagittal axis, and forward and backward around the vertical axis. Circular motion is possible around these two axes. The articular capsule is strengthened by bundles of the anterior and posterior sternoclavicular ligaments, interclavicular and costoclavicular ligaments.
The blade connects to chest with the help of muscles. This type of connection is called synsarcosis.
Connections of the free upper limb. This group includes the connections of the bones of the free upper limb with the girdle of the upper limb ( shoulder joint), as well as the own connections of the free upper limb.
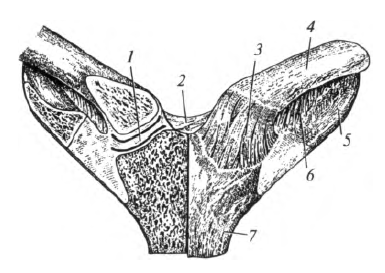
Shoulder joint, articulatio humeri, formed by the head of the humerus and the glenoid cavity of the scapula. The glenoid cavity is complemented by the articular lip (Fig. 5.6).
The joint capsule is attached to the scapula along the edge of the articular labrum, and on the humerus - along anatomical neck, wherein both tubercles remain outside the joint cavity.
Rice. 5.5. Sternoclavicular joint: 1 - articular disc; 2 - interclavicular ligament; 3 - anterior sternoclavicular ligament; 4 - collarbone; 5 - 1st rib; 6 - costoclavicular ligament; 7 - sternum
The capsule of the shoulder joint is strengthened by the coracobrachial and articular-brachial ligaments. The coracobrachial ligament starts from the coracoid process and is woven into the capsule from the superior and posterior sides. The articular-brachial ligaments are located in the thickness of the joint capsule.The shoulder joint is a typical spherical, multi-axial shape. This is the most mobile joint of all discontinuous joints. Movements in the shoulder joint are performed in all directions: around the frontal axis - flexion and extension; around the sagittal axis - abduction and adduction; around the vertical axis - rotation of the shoulder in and out; when moving from one axis to another - circular motion. The tendon of the long head of the biceps brachii muscle passes through the joint cavity.
elbow joint, articulatio cubiti, formed by three bones: humerus, ulna and radius. Three simple joints are formed between them: the humeroulnar, brachioradial and proximal radial joints. elbow (Fig. 5.7).
Rice. 5.6. Shoulder joint: 1 - tendon of the biceps brachii; 2 - head of the humerus; 3 - articular cavity of the scapula; 4 - labrum; 5 - axillary bursa
All three joints have a common capsule and one articular cavity, and therefore are combined into one (complex) joint. The articular surfaces are covered with hyaline cartilage.
shoulder joint, articulatio humeroulnaris, formed by the trochlea of the humerus and the trochlear notch of the ulna. The joint is helical or cochlear in shape, uniaxial.
humeral joint, articulatio humeroradialis, formed by the head of the condyle of the humerus and the glenoid fossa of the head radius. The joint is spherical in shape.
Proximal radioulnar joint, articulatio radioulnaris proximalis, formed by the articulation of the head of the radius and the radial notch of the ulna. The joint is cylindrical in shape.
All three joints are covered by one common articular capsule, which covers the ulnar, radial and coronoid fossae of the humerus, leaving the epicondyles free. In the lateral sections, the joint capsule is strengthened by strong radial and ulnar collateral ligaments. The head of the radius is surrounded by an annular ligament.
Around the frontal axis, flexion and extension of the forearm occurs at the humeroulnar and humeroradial joints. The first of them functions as a screw-shaped (a type of trochlear) joint. Due to the fact that the axis of the humerus trochlea passes obliquely in relation to the length of the shoulder, when flexed, the distal part of the forearm deviates slightly to the medial side - the hand rests not on the shoulder joint, but on the chest.
Rice. 5.7. Elbow joint: 1 - brachial bone; 2 - proximal radioulnar joint; 3 - ulnar collateral ligament; 4 - humeral-elbow joint; 5 - ulna; 6 - interosseous membrane of the forearm; 7- radius bone; 8 - tendon of the biceps brachii; 9- annular ligament of the radius; 10 - radial collateral ligament; I - humeroradial joint.
This is a functionally advantageous position for the upper limb, which must be created during first aid for fractures of the bones of the upper limb.
The humeroradial joint is spherical in shape, but in fact movements occur in it around the frontal axis: flexion and extension; around a vertical axis - rotation in and out (pronation and supination). Rotation occurs simultaneously in the proximal radioulnar (cylindrical) joint. There is no lateral movement in the humeroradial joint due to the presence of an interosseous membrane.
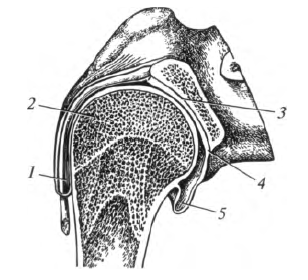
Connections of the bones of the forearm. The epiphyses of the ulna and radius are connected to each other by the proximal and distal radioulnar joints (Fig. 5.8). The interosseous membrane of the forearm (syndesmosis) is stretched almost along the entire length between these bones. It connects both bones of the forearm without interfering with movements in these joints.
As already noted, the proximal radioulnar joint is part of the elbow joint. The distal radioulnar joint is an independent cylindrical joint: the articular fossa in it is located on the radius, and the head is on the ulna.
The proximal and distal radioulnar joints function together to form a combined rotator cuff joint. Movement around the vertical axis is performed by the radius bone together with the hand. In this case, the ulna remains motionless.
Rice. 5.8. Connections of the bones of the forearm: 1 - proximal radioulnar joint; 2 - trochlear notch of the ulna; 3 - oblique chord; 4 - ulna; 5 - distal radioulnar joint; 6 - triangular disk; 7 - carpal articular surface; 8 - radius; 9 - interosseous membrane of the forearm; 10 - tendon of the biceps brachii; 11 - annular ligament of the radius
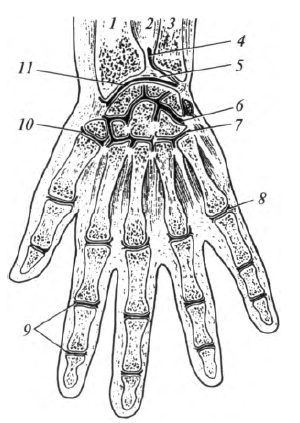
Rice. 5.9. Connections of the bones of the hand: 1 - radius; 2 - interosseous membrane of the forearm; 3 - ulna; 4 - distal radioulnar joint; 5 - triangular disk; 6 - midcarpal joint; 7 - carpometacarpal joints; 8 - metacarpophalangeal joint; 9 - interphalangeal joints; 10th metacarpophalangeal joint thumb; 11 - wrist joint
Wrist joint, articulatio radiocarpalis, form: the carpal articular surface of the radius, supplemented with medial side articular (triangular) disc, and articular surfaces of the proximal row of carpal bones, except for the pisiform (Fig. 5.9). The named bones of the wrist are firmly connected to each other by interosseous ligaments, and therefore form a single articular surface. The articular disc is triangular in shape, grows into the radius and separates the head of the ulna from the bones of the wrist, so the ulna does not participate in the formation of the wrist joint.
The joint is ellipsoidal. Around the frontal axis it performs flexion and extension, around the sagittal - abduction and adduction, and when moving from axis to axis - circular (conical) movement.
The joint capsule is strengthened on both sides, respectively, by the radial and ulnar collateral ligaments of the wrist. The palmar and dorsal radiocarpal ligaments are located on the palmar and dorsal surfaces of the joint.
Connections of the bones of the hand. In accordance with the classification of the bones of the hand, the following main joints are distinguished: between the bones of the proximal and distal rows of the wrist - the midcarpal joint; between the individual bones of the proximal and distal rows of the wrist - intercarpal joints; between the bones of the distal row of the wrist and the bones of the metacarpus - carpometacarpal joints; between the bones of the metacarpus and the proximal phalanges - metacarpophalangeal joints; between the proximal and middle, middle and distal phalanges - interphalangeal joints.
Midcarpal joint, articulatio mediocarpalis, located between the proximal (except for the pisiform) and distal radii of the carpal bones. The articulating surfaces of this joint form an S-shaped joint space, reinforced by powerful ligaments, so it is inactive.
Intercarpal joints, articulationes intercarpales, are located between the individual bones of the proximal or distal rows of the wrist. They are formed by the surfaces of articulating bones facing each other, flat in shape. Interosseous ligaments firmly attach the bones of the distal row of the wrist to each other, so that there is no movement between them. The pisiform bone forms its own connection (joint) with the triquetral bone.
It should be noted that the wrist and midcarpal joints functionally constitute one combined joint - the hand joint, articulatio manus. The proximal rad of the carpal bones in this joint plays the role of a bone disc.
Carpometacarpal joints, articulationes carpometacarpales, are the connections of the bones of the distal wrist with the bases metacarpal bones. In this case, the joint of the thumb is separate, and the rest have a common articular cavity and capsule, which is strengthened by the dorsal and palmar carpometacarpal ligaments. They are flat and inactive. All four bones of the second wrist and metacarpals II - V are very firmly connected to each other and mechanically form a solid base of the hand.
The formation of the carpometacarpal joint of the first finger involves the trapezium bone and the first metacarpal bone, which have a saddle shape. Movements in it occur around two axes. Around the frontal axis, the thumb flexes and extends along with the metacarpal bone; when flexed, the thumb moves towards the palm, opposed to the other fingers (opposition), and returns to its original position. Around the sagittal axis, the thumb is abducted and adducted to the index finger. As a result of a combination of movements around the two named axes, circular movement is possible in the joint.
On the palmar and dorsal surfaces of the hand there are numerous ligaments that connect the bones of the wrist, as well as the bones of the wrist with the bases of the metacarpal bones. They are especially well expressed on the palmar surface, forming a strong radiate ligament of the wrist.
Connections of the finger bones. Metacarpophalangeal joints, articu-lationes metacarpophalangeae, formed by the heads of the metacarpal bones and the fossae of the bases of the proximal phalanges. Collateral ligaments are located on the lateral sides of these joints. On the palmar surface there are stronger palmar ligaments. The deep transverse metacarpal ligament connects the heads of the II - V metacarpal bones, preventing them from diverging to the sides, strengthening the solid base of the hand.
In form II-IV, the metacarpophalangeal joints are spherical. Around the frontal axis they perform flexion and extension, around the sagittal axis - abduction of the fingers, as well as circular movements. Movements around the vertical axis in these joints are not realized due to the absence of rotator muscles.
The metacarpophalangeal joint of the thumb is block-shaped in shape. The palmar part of the joint capsule contains two sesamoid ossicles (lateral and medial). It undergoes flexion and extension around the frontal axis.
interphalangeal joints, articulationes interphalangeae, are located between the proximal and middle, middle and distal phalanges of the II - V fingers, as well as between the proximal and distal phalanges of the first finger. The capsule is strengthened by palmar and lateral (collateral) ligaments, which exclude the possibility of lateral movements. Block-shaped joints. Movements in them are carried out only around the frontal axis: flexion and extension of the phalanges.
5.5. Bone connections lower limb
Connections of the bones of the lower limb girdle. The pelvic bones are connected to each other and to the sacrum through discontinuous, continuous joints and semi-joints.
Sacroiliac joint, articulatio sacroiliaca, formed by the ear-shaped surfaces of the sacrum and ilium. The articular surfaces are covered with fibrous cartilage. The sacroiliac joint is flat, strengthened by powerful sacroiliac ligaments, so there is no movement in it.
pubic symphysis, symphysis pubica, located in the median plane, connects the pubic bones to each other and is a semi-joint (Fig. 5.10). Inside the cartilage (in its upper-posterior section) there is a cavity in the form of a narrow gap, which develops in the 1st - 2nd year of life. Small movements in the pubic symphysis are possible only in women during childbirth. The pubic symphysis is strengthened by two ligaments: from above - by the superior pubic ligament, from below - by the inferior pubic ligament.
Continuous connections of the pelvic bone. The iliolumbar ligament descends from transverse processes two lower lumbar vertebrae to the iliac crest.
Sacrotuberous ligament connects the ischial tuberosity with the lateral edge of the sacrum and coccyx.
Sacrospinous ligament stretched from the ischial spine to the lateral edge of the sacrum.
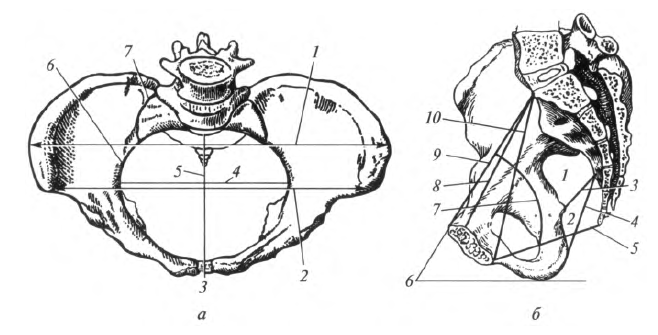
Rice. 5.10. Bone connections and pelvic dimensions (diagram): a - top view: 7 - distantia intercristalis; 2 - distantia interspinosa; 3 - pubic symphysis; 4 - transverse size of the entrance to the pelvis; 5 - true conjugate; 6 - border line; 7 - sacroiliac joint; b - side view: 7 - greater sciatic foramen; 2 - lesser sciatic foramen; 3 - sacrospinous ligament; 4 - sacrotuberous ligament; 5 - exit conjugate; 6 - pelvic tilt angle; 7 - wire axis of the pelvis; 8 - true conjugate; 9 - anatomical conjugate; 10 - diagonal conjugate
Obturator membrane closes the hole of the same name, leaving free a small hole at the obturator groove (see Fig. 5.11).The pelvis as a whole. Pelvic bones, sacrum, coccyx and belonging to them ligamentous apparatus form the pelvis, pelvis. With the help of the pelvic bones, the torso is also connected to the free part of the lower extremities.
Distinguish big basin, pelvis major, and pelvis, pelvis minor. They are separated from each other by a boundary line, which is drawn on both sides of the promontory through an arcuate line along the pubic crest to the pubic tubercle and then along the upper edge of the pubic symphysis.
The walls of the pelvic cavity form: at the back - the sacrum and the anterior surface of the coccyx; in front - the anterior sections of the pubic bones and symphysis; from the sides - the inner surface of the pelvic bone below the boundary line. The obturator foramen located here is almost entirely covered by the membrane of the same name, except for a small hole in the area of the obturator groove.
On the lateral wall of the pelvis there are the greater and lesser sciatic foramina. The greater sciatic foramen is bounded by the sacrospinous ligament and the greater sciatic notch. The lesser sciatic foramen is bounded by the sacrospinous and sacrotuberous ligaments, as well as the lesser sciatic notch. Through these openings from the pelvic cavity to gluteal region vessels and nerves pass through.
When a person is in an upright position, the pelvis is tilted forward; the plane of the upper aperture of the pelvis forms sharp corner with a horizontal plane, forming an angle of inclination of the pelvis. For women this angle is 55-60°, for men 50-55°.
Sexual differences in the pelvis. Women have a lower and wider pelvis. Distance between awns and ridges iliac bones more, since the wings of these bones are turned to the sides. The promontory protrudes forward less, so the entrance to the male pelvis resembles a card heart in shape; in women it is more rounded, sometimes even approaching an ellipse. Symphysis female pelvis wider and shorter. The pelvic cavity in women is wider, in men it is narrower. The sacrum in women is wider and shorter, ischial tuberosities turned to the sides, so the transverse size of the outlet is 1 - 2 cm larger. Angle between lower branches pubic bones(subpubic angle) in women is 90-100°, in men 70-75°.
In obstetrics, knowledge of the average size of a woman’s pelvis is of great importance for predicting the course of labor. The median anteroposterior dimensions of the small pelvis are common name conjugate Typically, input and output conjugates are measured. The direct size of the entrance to the pelvis - the distance between the promontory and the upper edge of the pubic symphysis - is called the anatomical conjugate. It is equal to 11.5 cm. The distance between the promontory and the most posteriorly protruding point of the symphysis is called the true, or gynecological conjugate; it is equal to 10.5 - 11.0 cm. The diagonal conjugate is measured between the promontory and the lower edge of the symphysis; it can be determined in a woman when vaginal examination; its size is 12.5 -13.0 cm. To determine the size of the true conjugate, it is necessary to subtract 2 cm from the length of the diagonal conjugate.
Transverse diameter of the inlet to the pelvis measured between the most distant points of the boundary line; it is equal to 13.5 cm. The oblique diameter of the entrance to the small pelvis is the distance between the sacroiliac joint on one side and the iliopubic eminence on the other; it is 13 cm.
The direct size of the outlet (outlet conjugate) from the pelvis in women is 9 cm and is determined between the apex of the coccyx and the lower edge of the pubic symphysis. During childbirth, the coccyx deviates back in sacrococcygeal synchondrosis, and this distance increases by 2.0 -2.5 cm.
Transverse outlet size from the pelvic cavity is 11 cm. It is measured between the inner surfaces of the ischial tuberosities.
Wired pelvic axis, or a leading line, is a curve connecting the midpoints of all conjugates. She's almost on her way parallel to the anterior surface of the sacrum and shows the path that the fetal head takes during childbirth.
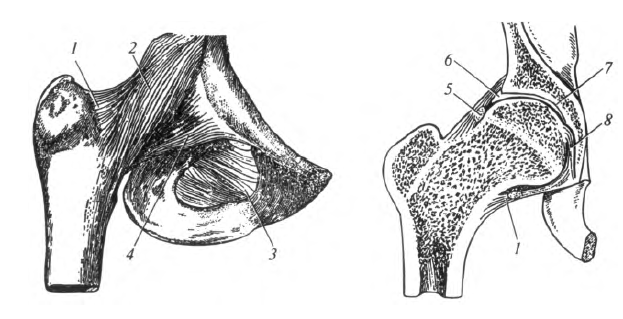
Rice. 5.11. Hip joint: 1 - joint capsule; 2- iliofemoral ligament; 3- obturator membrane; 4- pubofemoral ligament; 5 - circular zone; 6- articular lip; 7 - acetabulum; 8- bunch of heads femur
In obstetric practice great importance They also have some dimensions of the large pelvis (see Fig. 5.10): the distance between the anterior superior iliac spines (distantia interspinosa), which is 25 - 27 cm; the distance between the most distant points of the iliac crests (distantia intercristalis), equal to 27 - 29 cm; the distance between the greater trochanters of the femurs (distantia intertrochanterica), equal to 31-32 cm. To assess the anteroposterior dimensions of the pelvis, the external conjugate is measured - the distance between the outer surface of the pubic symphysis and spinous process V lumbar vertebra, which is 20 cm.Connections of the free lower limb.
Hip joint, articulatio coxae, is formed by the acetabulum of the pelvis and the head of the femur (Fig. 5.11). The hole in the center acetabulum filled with adipose tissue.
The articular capsule is attached along the edge of the acetabular labrum and along the medial edge of the femoral neck. Thus, most of The femoral neck lies outside the joint cavity and the fracture of its lateral part is extra-articular, which significantly facilitates the treatment and prognosis of the injury.
In the thickness of the capsule there is a ligament called the circular zone, which covers the neck of the femur approximately in the middle. The joint capsule also contains fibers of three ligaments directed longitudinally: the iliofemoral, pubofemoral and ischiofemoral, connecting the bones of the same name.
The following elements of the joint are auxiliary: the acetabulum, which complements the lunate articular surface of the acetabulum; transverse acetabular ligament, thrown over the acetabular notch; ligament of the femoral head connecting the fossa of the acetabulum with the fossa of the femoral head and containing blood vessels, which nourish the head of the femur.
The hip joint is a type of ball-and-socket joint - nut-shaped, or cup-shaped. It allows movements around all axes: flexion and extension around the frontal axis, abduction and adduction around the sagittal axis, circular movement around the frontal and sagittal axes, rotation around the vertical axis.
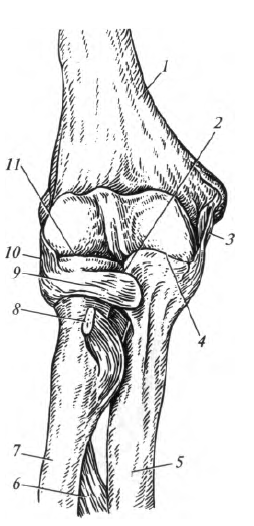
Knee-joint, articulatio genus, - most large joint human body. Three bones take part in its formation: the femur, tibia and patella (Fig. 5.12). The articular surfaces are: the lateral and medial condyles of the femur, the superior articular surface of the tibia and the articular surface of the patella.
The capsule of the knee joint is attached to the femur 1 cm above the edge of the articular cartilage and anteriorly passes into the suprapatellar bursa, located above the patella between the femur and the tendon of the quadriceps femoris muscle. On the tibia, the capsule is attached along the edge of the articular surface.
The joint capsule is strengthened by the fibular and tibial collateral ligaments, located on both sides of the joint, as well as the patellar ligament. It is a tendon of the quadriceps femoris muscle located below the patella.
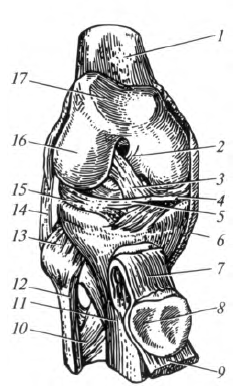
Rice. 5.12. Knee-joint: 1 - femur; 2 - posterior cruciate ligament; 3 - anterior cruciate ligament; 4 - medial meniscus; 5 - transverse ligament of the knee; 6- collateral tibial ligament; 7- patellar ligament; 8 - patella; 9 - quadriceps tendon; 10 - interosseous membrane of the leg; eleven - tibia; 12 - fibula; 13 - tibiofibular joint; 14 - collateral fibular ligament; 15 - lateral meniscus; 16 - lateral condyle of the femur; 17 - patellar surface
The joint has many auxiliary elements, such as the patella, menisci, intraarticular ligaments, bursae and folds.
The lateral and medial menisci partially eliminate the incongruity of the articular surfaces and play a shock-absorbing role. The medial meniscus is narrow, semilunar in shape. The lateral meniscus is wider and oval. The menisci are connected to each other by the transverse knee ligament.
The anterior and posterior cruciate ligaments firmly connect the femur and tibia, crossing over each other in an "X" shape.
The auxiliary elements of the knee joint also include pterygoid folds, which contain fatty tissue. They
located below the patella on both sides. An unpaired infrapatellar synovial fold runs from the apex of the patella to the anterior part of the tibia.
The knee joint has several synovial bursae, bursae synoviales, some of which communicate with the joint cavity:
1) suprapatellar bursa, located between the femur and the tendon of the quadriceps femoris muscle; communicates with the joint cavity;
2) deep subpatellar bursa, located between the patellar ligament and the tibia;
3) subcutaneous and subtendinous prepatellar bursae, located in the tissue on the anterior surface of the knee joint;
4) muscle bags located at the attachment point of the leg and thigh muscles in the area of the knee joint.
Rice. 5.13. Joints of the shin bones: 1 - upper articular surface; 2 - tibia; 3 - interosseous membrane of the leg; 4 - medial malleolus; 5 - lower articular surface; b - lateral malleolus; 7 - tibiofibular syndesmosis; 8 - fibula; 9 - tibiofibular joint
The shape of the knee joint is condylar. Flexion and extension occur around the frontal axis. Around the vertical axis in a bent position, rotation of the lower leg is possible to a small extent.
Joints of the leg bones. The bones of the lower leg are connected to each other using discontinuous and continuous connections.
The proximal ends of the bones of the lower leg are connected by a discontinuous connection - the tibiofibular joint, articulatio tibiofibularis (Fig. 5.13), - flat, inactive. Connects the distal ends of the leg bones tibiofibular syndesmosis, represented by short ligaments connecting the fibular notch of the tibia and the lateral malleolus of the fibula. A strong fibrous plate - an interosseous membrane - connects both bones almost along its entire length.
Connections of the bones of the foot. The joints of the foot bones can be divided into four groups:
1) connections of the bones of the foot with the bones of the lower leg - ankle joint;
2) connections between the bones of the tarsus;
3) connections between the bones of the tarsus and metatarsus;
4) connections of the finger bones.
Ankle (supratalar) joint, articulatio talocruralis, formed by both bones of the tibia and the talus (Fig. 5.14). In this case, the block of the talus is covered from the lateral sides by the lateral and medial ankles.
The joint capsule is attached along the edge of the articular surfaces. On the medial side it is strengthened by the medial (deltoid) ligament. On the lateral side, the joint capsule is strengthened by three ligaments: anterior and posterior early-fibular, as well as calcaneofibular, which connect the corresponding bones.
Rice. 5.14. Connections of the bones of the foot: 1 - tibia; 2 - interosseous membrane of the leg; 3 - fibula; 4 - ankle joint; 5 - talocalcaneal-navicular joint; 6 - scaphoid; 7 - calcaneocuboid joint; 8 - tarsometatarsal joints; 9 - metatarsophalangeal joints; 10 - interphalangeal joints
The ankle joint is block-shaped in shape. It allows movements around the frontal axis: plantar flexion and dorsiflexion (extension). Due to the fact that the trochlea of the talus is narrower at the back, with maximum plantar flexion in ankle joint lateral rocking movements are possible in a small volume. Movements in the ankle joint are combined with movements in the subtalar and talocaleonavicular joints.
Joints of the tarsal bones. Presented the following joints: subtalar, talocaleonavicular, calcaneocuboid, cuneonavicular.
subtalar joint, articulatio subtalaris, located between the talus and calcaneal bones. The joint is cylindrical; minor movements are possible only around the sagittal axis.
talocaleonavicular joint, articulatio talocalcaneo-navicularis, has a spherical shape, located between the bones of the same name. The glenoid cavity is supplemented by cartilage, which is formed along the plantar calcaneonavicular ligament.
Ankle (supratalar), The subtalar and talocaleonavicular joints usually function together, forming a single functional joint of the foot, in which the talus plays the role of a bone disc.
calcaneocuboid joint, articulatio calcaneocuboidea, located between the bones of the same name, saddle-shaped, inactive.
From a surgical point of view, the calcaneocuboid and talonavicular (part of the talocaleonavicular) joints are considered as one joint - the transverse tarsal joint (Shopard joint). The articular cleft of these joints is located almost on the same line, along which it is possible to isolate (exarticulate) the foot in case of severe damage.
Wedge-navicular joint, articulatio cuneonavicularis, is formed by the scaphoid and sphenoid bones and is practically motionless.
Tarsometatarsal joints, articulationes tarsometatarsales, are three flat joints located between the medial cuneiform and first metatarsal bones; between the intermediate, lateral cuneiform and II, III metatarsal bones; between the cuboid and IV, V metatarsal bones. From a surgical point of view, all three joints are combined into one joint - the Lisfranc joint, which is also used to isolate the distal part of the foot.
metatarsophalangeal joints, articulationes metatarsophalangeae, formed by the heads of the metatarsal bones and the fossae of the bases of the proximal phalanges. They are spherical in shape, strengthened by collateral (lateral) and plantar ligaments. They are fixed to each other by a deep transverse metatarsal ligament that runs transversely between the heads of the 1st and 5th metatarsal bones. This ligament plays an important role in the formation of the transverse metatarsal arch of the foot.
The plantar part of the capsule of the first metatarsophalangeal joint is permanently enclosed by two sesamoid bones, so it functions as a trochlear joint. The joints of the remaining four fingers function as ellipses. They allow flexion and extension around the frontal axis, abduction and adduction around the sagittal axis, and, to a small extent, circular movement.
interphalangeal joints, articulationes interphalangeae, are similar in shape and function to the same joints of the hand. They belong to the block joints. They are strengthened by collateral and plantar ligaments. In the normal state, the proximal phalanges are in a state of dorsiflexion, and the middle ones are in plantar flexion.
As mentioned earlier, the foot forms longitudinal (five) and transverse (two) arches. Special role in fixation of the transverse arches, it belongs to the deep transverse metatarsal ligament, which connects the metatarsophalangeal joints. The longitudinal arches are strengthened by a long plantar ligament, which runs from the calcaneal tubercle to the base of each metatarsal. Ligaments are “passive” fixators of the arches of the foot.
Control questions
1. What types of bone joints do you know?
2. Describe continuous connections bones.
3. Name the main elements of the joint.
4. List the auxiliary elements of the joint.
5. How are joints classified by shape? Describe possible movements in them.
6. Give a classification of vertebral connections.
7. List the curves of the spinal column and name the timing of their appearance.
8. What rib connections do you know?
9. Describe the structural features of the temporomandibular joint.
10. List the joints of the upper limb. What movements are implemented in them?
11. What compounds does it form? hip bone?
12. What gender differences do you know in the pelvis?
13. List the dimensions of the female pelvis.
14. Describe the joints of the free lower limb.
Continuous bone connections- earlier in development. They are characterized by significant strength, little flexibility, little elasticity and limited movement. Continuous bone connections, depending on the structure of the tissue that connects them, are divided into three types of synarthrosis (BNA).
1. Fibrous compounds, junctura fibrosa s. syndesmosis.
2. Cartilaginous joints, junctura cortilaginea s. synchondrosis.
3. Bone joints of Junctura ossea s. synostosis.
Fibrous compounds are formed after the birth of a child when there remains between the bones, which ensures the connection of the bones.
1 TO fibrous compounds(syndesmoses) include: interosseous membranes, membranae interosseae, ligaments, ligamenta, interosseous sutures, suturae cranii, herniations, gomphosis and fontanelles, fonticuli.
Interosseous fibrous membranes, membrana interossea fibrosae, connect adjacent bones. They are located between the bones of the forearm, membrana interossea antebrachii, and between the bones of the lower leg, membranae interosseae cruris, or cover holes in the bones: for example, the obturator foramen membrane, membranae obturatoria, the anterior and posterior atlanto-occipital membranes, membranae atlantooccipitalis anterior et posterior. Interosseous membranes connect bones and form large surface to attach muscles to them. They are formed predominantly by bundles of collagen fibers and have openings for the passage of blood vessels and nerves.
Ligaments, ligamenta, serve to secure bone joints. They can be very short, such as the dorsal intercarpal ligament, ligg. intercarpalia dorsalia, or, conversely, long, like the anterior and posterior longitudinal ligaments of the spinal column, ligg. longitudinale anterius et posterius.
Ligaments are strong fibrous cords consisting of longitudinal, oblique and crossed bundles of collagen and a small amount of elastic fibers. Ligaments can withstand high tensile loads. This group also includes ligaments formed only by elastic fibers. They are not as strong as fibrous syndesmoses, but very stretchy and flexible. These are the yellow ligaments, liggamenta flavae, which are located between the vertebral arches.
Interosseous sutures, suturae cranii occur only in the skull; they are a type of syndesmosis, in which the edges of the bones are firmly connected by small layers of fibrous connective tissue. The seams are characterized by extreme strength. Depending on the shape of the skull bones, the following sutures are distinguished:
- Serrated, sutura serrata s. dentata (BNA), in which the edge of one bone has teeth that fit into the recesses of the second bone (for example, at the connection frontal bone with parietal);
- Scaly, sutura squamosa, has the peculiarity that the pointed end of one bone in the form of scales is superimposed on the pointed edge of another bone (for example, a combination of scales of the temporal bone with the parietal);
- Flat, sutura plana s. harmonia (BNA), in which the smooth edge of one bone is adjacent to the same edge of the second, without the formation of protrusions, which is typical for the bones of the facial skull (for example, between the nasal bones).
Herniation [gomphosis], gomphosis, is a type of fibrous connection of bones. It can be observed between the roots of the teeth and the dental cells (dental-collar junction, sindesmosis dento-alveolaris). Between the tooth and the bone tissue of the cell there is a layer of connective tissue - periodontium, periodontium.
2. B cartilage joints(synchondrosis) - the bones are combined with a layer of fibrous or hyaline cartilage. Hyaline cartilage harmoniously combines strength and elasticity. Synchondroses are quite strong and elastic, due to which they perform spring functions. The mobility of this connection is insignificant and depends on the thickness of the cartilaginous layer - the greater its thickness, the higher the mobility, and vice versa. An example of synchondrosis formed by fibrous cartilage is intervertebral discs, discus intewertebrales, located between the vertebral bodies. They are strong and elastic, serving as a buffer during shocks and shocks. An example of synchondrosis formed by hyaline cartilage is the epiphyseal cartilage, located on the border of the epiphyses and metaphyses in long tubular bones, or the costal cartilages, connecting the ribs to the sternum. According to the duration of their existence, synchondrosis can be: temporary, existing until a certain age (for example, the cartilaginous connection of the diaphysis and epiphyses of long tubular bones and three pelvic bones), as well as permanent, remaining throughout a person’s life (for example, between the pyramid of the temporal bone and neighboring bones : sphenoid and occipital). A type of synchondrosis is the pubic symphysis, symphysis pubica. It also combines bones with the help of cartilage small cavity.
3. If a temporary continuous connection (fibrous or cartilaginous) is replaced by bone tissue, it is called synostosis (BNA). This type of connection is the most durable, but loses its elastic function. An example of synostosis in an adult is the connection between the body of the occipital and sphenoid bones, between
1. Continuous– synarthrosis – between the bones there is a layer that connects tissue. Motionless.
2. Semi-continuous– hemiarthrosis (symphyses) – a small cavity with fluid
3. Intermittent– diarthrosis (joints) of the bones are displaced relative to each other
All types of joints in the spinal column
Continuous connections : whether there is a gap or cavity,
1.Fibrous joints(syndesmoses) – ligaments(throws from one bone to another), membranes– flat, wide, along the cord of bone – radius and ulna, hip joint– pelvic bone – obturator membrane – tibia and fibula; seams- skull - serrated suture, flat suture - facial bones, scaly suture - temporal region, hammering– attachment of teeth to the jaw; collagen - strength in the ligament, elastic fibers - mobility 2. Cartilaginous connections(synchodrosis) – permanent – sternum and 1 rib, intervertebral discs, temporary - pelvis - ischial, pubic, iliac, sacrum, attachment points of the epiphysis and diaphysis 3. Bone connections(synostosis) – replacement of temporary cartilaginous joints – fused sacrum
Intermittent connections = joints. mandatory and auxiliary elements. Required: 1.Articular parts - in- and congruent, covered with hyaline cartilage - smoothes bone tissue, as dense as the bone itself, it greatly facilitates movement in the joint. 2.Articular capsule– fibrous (protects the joint) and synovial membranes (rich in blood vessels, produces synovial fluid). 3.Articular cavity– slit-like space between the articular surfaces, contains synovial fluid. 4. Synovial fluid – secreted by a membrane, with exfoliating cartilaginous and flat connective tissue cells form mucus, promotes adhesion, wetting, facilitating gliding
Semi-continuous = Half-joint – fibrous or cartilaginous joints. Symphysis pubis, manubrium sternum, intervertebral. There is no capsule, the inner surface of the fissure is not lined with synovial membrane. Can be strengthened by interosseous ligaments
10. Continuous bone connections. Classification. Examples.
Continuous connections: synarthrosis - between the bones there is a layer of tissue connecting. Fixed, no gap or cavity.
ligaments (spreads from one bone to another) - collagen fibers, low extensibility, very strong,
membranes – flat, wide, along the cord of bone – radius and ulna, hip joint – pelvic bone – obturator membrane – tibia and fibula;
sutures - skulls - serrated suture, flat suture - bones of the facial skull, scaly suture - temporal and parietal regions, sutures - shock absorption zones and shocks when walking, jumping. Also serve as areas for bone growth.
impaction – connection of the tooth root with the walls of the alveoli.
Fibrous compounds (syndesmoses) –
Cartilaginous joints (synchodrosis) are strong and elastic - permanent - sternum and 1 rib, intervertebral discs, temporary - pelvis - ischial, pubic, iliac, sacrum, attachment points of the epiphysis and diaphysis
Bone joints (synostoses) – replacement of temporary cartilaginous joints
11.Joint structure.
1. Simple joints - formed by only 2 surfaces
2. Complex joints - in the formation of more than 2 articular surfaces - elbow joint, wrist, knee, ankle
3. complex joint - the presence of any other tissue - intra-articular disc or meniscus - bone-cartilage-bone
MANDATORY: - articular (hyaline) cartilage– smooth out bone tissue. As dense as the bone itself, it greatly facilitates movement in the joint. Articular cartilage does not contain nerve endings and blood vessels. Cartilage receives nutrition from synovial fluid. Cartilage consists of special cartilaginous cells - chondrocytes and intercellular substance - matrix. The matrix includes loosely arranged connective tissue fibers - the main substance of cartilage. The special structure makes cartilage look like a sponge - in calm state it absorbs fluid, and when loaded, squeezes it into the joint cavity, providing, as it were, additional “lubrication” of the joint. - joint capsule or capsule- a closed cover that surrounds the ends of connecting bones and passes into the periosteum of these bones. This capsule consists of two layers called membranes. Outer membrane (fibrous) – the protective covering of the joint and ligaments that control and support the joint, preventing displacement. Internal (synovial) - produces synovial fluid - articular (synovial) cavity- this is a sealed space between the inner membrane of the articular capsule and the surfaces of the connecting bones. - synovial fluid - viscoelastic joint lubricant (hyaluronic acid). It washes the articular surfaces of the bones, nourishes the articular cartilage, acts as a shock absorber, and also affects the mobility of the joint as its viscosity changes.
AUXILIARY Articular discs and menisci – cartilaginous plates of various shapes in incongruent joints. Shift when moving. They smooth out the articulating surfaces, contour them, and absorb shocks and jolts during movement. Articular lips– along the edge of the concave articular surface, deepen and complement it. Synovial bursae and vagina– protrusions of the synovial membrane in thinned areas of the fibrous membrane of the joint. Eliminate friction of contacting tendons and bones. Ligaments –(hip, knee) – covered with a synovial membrane – strengthening the joint.
![]()
All bone connections can be divided into two groups: a) continuous connections, earlier in development in phylogeny, immobile or inactive in function; b) discontinuous connections, later in development and more mobile in function. Between these forms there is a transitional one - from continuous to discontinuous or vice versa - half-joint.
The continuous connection of bones is carried out through connective tissue, cartilage and bone tissue (the bones of the skull itself). A discontinuous bone connection, or joint, is a younger formation of a bone connection. All joints have a general structural plan, including the articular cavity, articular capsule and articular surfaces.
The articular cavity is distinguished conditionally, since normally there is no void between the articular capsule and the articular ends of the bones, but there is liquid.
The articular capsule covers the articular surfaces of the bones, forming an airtight capsule. The joint capsule consists of two layers, outer layer which passes into the periosteum. Inner layer releases fluid into the joint cavity, which acts as a lubricant, ensuring free sliding of the articular surfaces.
The articular surfaces of articulating bones are covered with articular cartilage. The smooth surface of articular cartilage promotes movement in the joints. Articular surfaces are very diverse in shape and size; they are usually compared with geometric shapes. Hence the name of the joints according to their shape: spherical (shoulder), ellipsoid (radio-carpal), cylindrical (radio-ulnar), etc. Since the movements of the articulating links are performed around one, two or many axes, joints are also usually divided into multi-axial (spherical ), biaxial (ellipsoidal, saddle-shaped) and uniaxial (cylindrical, block-shaped).
Depending on the number of bones that articulate, joints are divided into simple, in which two bones are connected, and complex, in which more than two bones are articulated.










